Introduction
An anorectal abscess refers to a collection of pus in the anal or rectal region. They are more common in men than in women and have high rates of recurrence. One third of patients with an anorectal abscess have an associated perianal fistula at the time of presentation.
Pathophysiology
Anorectal abscess are thought to be caused by plugging of the anal ducts, which drain the anal glands in the anal wall (which normally helping to ease the passage of faecal matter with mucus secretions). Blockage of an anal duct results in fluid stasis, which will lead to infection. Common causative organisms include E. coli, Bacteriodes spp., and Enterococcus spp.
The anal glands are located in the intersphincteric space (between the internal and external anal sphincters), therefore infection from the glands here spreads to adjacent areas. Anorectal abscesses can be categorised by the area (Fig. 1) in which they occur: (1) Perianal* (2) Ischiorectal (3) Intersphincteric (4) Supralevator
*The perianal area is the most common site of abscess formation
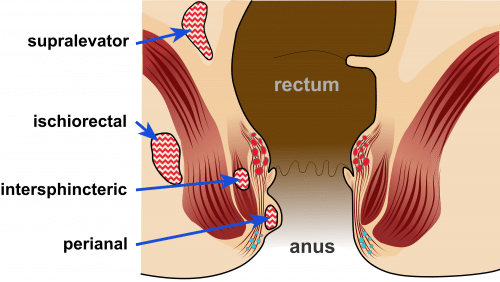
Figure 1 – Classification of anorectal abscess by location
Clinical Features
Anorectal abscesses present with severe pain in the perianal region, worse with direct pressure (i.e. when sat down), alongside potential perianal discharge or bleeding. Severe abscesses may present with systemic features* such as fever or rigors, general malaise, or other clinical features of sepsis.
On examination, there will be a erythematous, fluctuant, tender perianal swelling (Fig. 1), which may be discharging pus or have surrounding erythema and induration. Deeper abscesses may not have any obvious external signs, however they may present with severe tenderness on Digital Rectal Examination.
Investigations
The diagnosis is typically a clinical one. However, as the majority will require surgical intervention (see below), routine bloods (FBC, U&Es, clotting) are typically performed.
Patients with an anorectal abscess without any known fistula-in-ano or other rectal pathology should have their serum glucose or HbA1c sent to check for underlying diabetes mellitus.
For patients with atypical presentations or in those suspicious for deeper abscesses (i.e. ischiorectal or supralevator), complex perianal fistula, or perianal Crohn’s disease, then additional imaging is required where possible (ideally an MRI pelvis scan, however CT imaging can help diagnose deep abscesses in the acute setting if MRI is not available)
Management
Patients should be started on antibiotic therapy, as guided by local protocol, and provided with sufficient analgesia.
The main management* for anorectal abscesses is with an examination of the anorectum and incision and drainage (I&D) of the abscess, which should always be performed under general anaesthetic wherever possible.
These can be left to heal by secondary intention. Evidence has shown that whilst the wound can be packed for the first 24 hours to aid with haemostasis, there is no additional benefit to further repacking beyond that)
Intra-operative proctoscopy should be performed to check for the presence of any identifiable fistula-in-ano. This is also necessary to rule out other pathology such as malignant lesions. If a fistula is identified, the insertion of a seton can be considered, but only by experienced surgeons. This is because there is a risk of creating iatrogenic fistulae due to the infected tissues being very friable in the acute setting.
Limited data has suggested that use of post-operative antibiotics following drainage of anorectal abscess may lower the risk of fistula formation.
*In immunocompetent patients with a small perianal abscess and without systemic signs of sepsis, then rarely an antibiotic approach alone (i.e. without surgery) can be trialled
Key Points
- Anorectal abscess are caused by blockage of the anal ducts, resulting in stasis and bacterial flora overgrowth
- Diagnosis is typically clinical, however MRI imaging can be used in complicated or chronic disease
- Management is via incision and drainage followed by proctoscopy, and allow the wound to heal via secondary intention

