Introduction
Gastric cancer is the fifth most commonly diagnosed cancer globally and is the second highest cause of cancer-related deaths, mostly due to patients presenting with advanced disease.
The majority (>90%) of gastric cancers arise from the gastric mucosa as adenocarcinomas. The remainder are a mixture of connective tissue (i.e. GIST), lymphoid, or neuroendocrine malignancies.
In this article, we shall look the risk factors, clinical features and management of a patient with gastric adenocarcinoma.
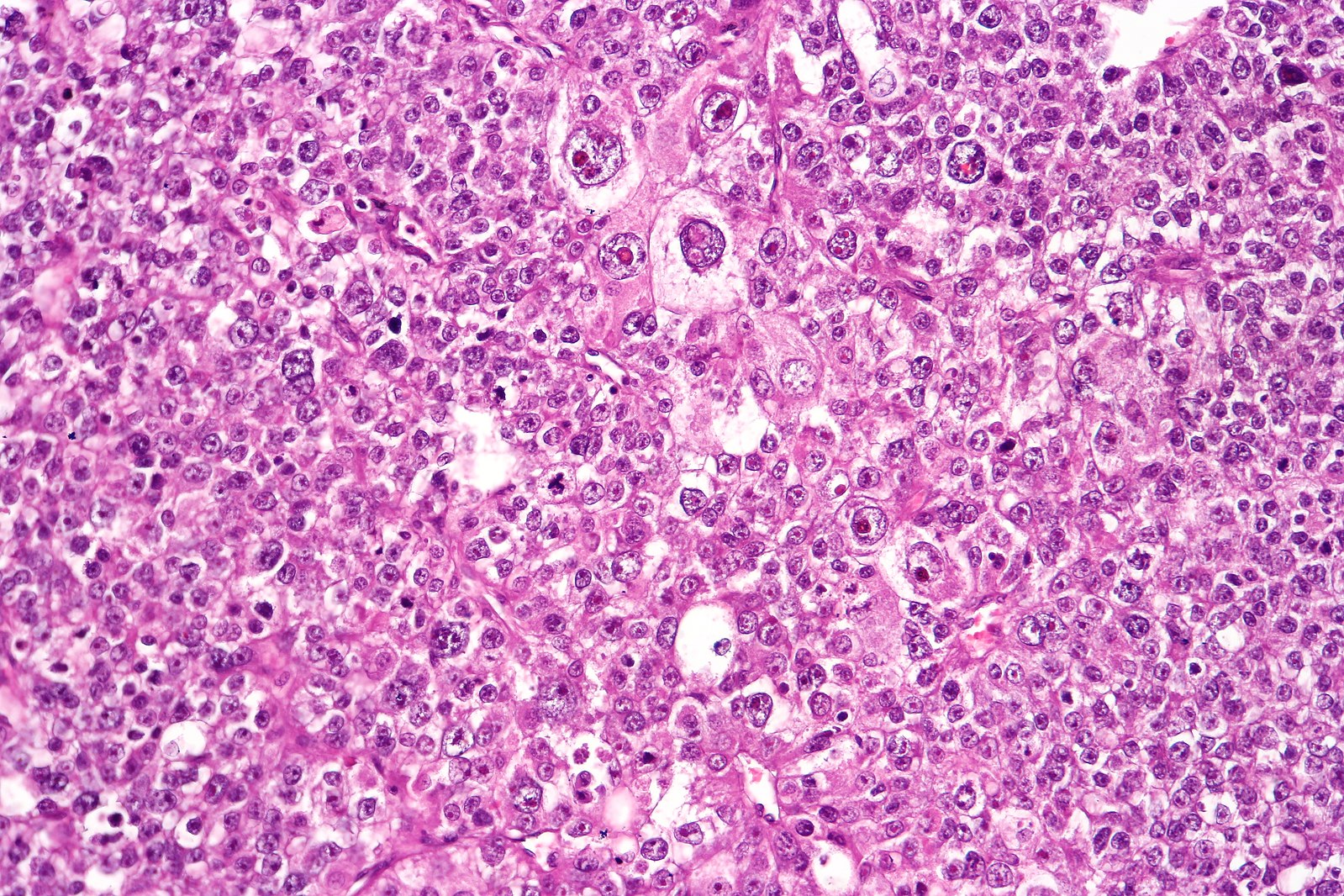
Figure 1 – A poorly differentiated gastric adenocarcinoma on histology
Risk Factors
In many countries, rates of gastric cancer have fallen in the past few decades (mainly due to an improved diet and treatment of Helicobacter Pylori infections), however it remains much more common in Far Eastern countries, such as Japan and Korea.
The major risk factors for developing gastric cancer include male gender, H. pylori infection*, increasing age, smoking, and alcohol consumption. Other risk factors include salt in diet, positive family history, and pernicious anaemia.
Helicobacter pylori and Gastric Cancer
The risk of gastric cancer is nearly six times higher for H. Pylori-infected inidividuals, than for uninfected individuals. However, whilst around 60% of the world’s population are infected with H. Pylori, less than 0.5% will develop gastric adenocarcinoma.
H. pylori infection causes acute gastritis (and then chronic gastritis), which can progress to metaplasia, to dysplasia, and then to cancer. While there is no clear evidence that H. Pylori eradication prevents gastric cancer, it does prevent the progression of precancerous lesions.
Clinical Features
The symptoms of gastric cancer are frequently vague and non-specific, with patients often unfortunately presenting at an advanced stage.
The common presenting symptoms include dyspepsia (particularly if new-onset or not responsive to simple PPI treatment), dysphagia, early satiety, vomiting, or melena. Non-specific cancer symptoms (anorexia, weight loss, or anaemia) are markers of late stage disease.
On examination, clinical signs are usually absent, especially in the early stages, however an epigastric mass may be felt in late stage disease. Troisier sign is the presence of a palpable left supraclavicular node (Virchow node) and is considered a sign of metastatic abdominal malignancy (typically gastric).
Other signs of metastatic disease include hepatomegaly, ascites, jaundice, or acanthosis nigricans (Fig. 2).

Figure 2 – Acanthosis nigricans, hyperpigmentation of the skin creases
Differential Diagnosis
Gastric cancer often presents with non-specific symptoms and consequently there are a wide range of potential differential diagnoses. Important diagnoses to consider include peptic ulcer disease, GORD, gallstone disease, and pancreatic cancer.
Investigations
Any patient presenting with clinical features of gastric cancer, including haematemesis or melena, will warrant urgent bloods, including a full blood count and liver function tests.
However, the primary investigation of any suspected gastric cancer is an urgent upper GI endoscopy* (OGD), allowing for the direct visualisation of any malignancy present (Fig. 3) and subsequent biopsies taken as needed.
Current NICE guidelines recommend referring for an urgent OGD for any patients presenting with new-onset dysphagia or aged >55 years presenting with weight loss and either upper abdominal pain, reflux, or dyspepsia.
Biopsies from suspected gastric malignancies should be sent for:
- Histology – for classification and grading of any neoplasia present
- CLO test – for the presence of H. Pylori
- HER2/neu protein expression – this will allow for targeted monoclonal therapies if present
*A CT scan may show thickening of the gastric wall but does not allow direct visualisation or biopsy, hence OGD is the only definitive means of diagnosis.
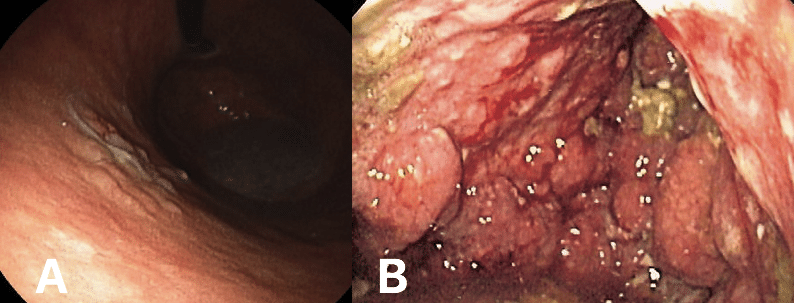
Figure 3 – (A) Early stage gastric cancer (B) Linitis Plastica, whereby the malignancy has invaded most of the stomach and produced a ‘leather-bottle’ type appearance
For staging and in order to plan treatment, all patients need a CT Chest-Abdomen-Pelvis scan* and a staging laparoscopy (to look for peritoneal metastases). The most commonly used staging system for gastric cancers is TNM staging.
*As gastric cancers are not very “PET avid” (do not take up the radioactive tracer well), PET scans are rarely used in staging gastric cancers.
Management
All patients should be discussed at a specialist upper GI cancer multi-disciplinary team meeting for definitive management plans (including potential palliation decisions)
Ensuring adequate nutrition is essential, therefore each patient should undergo nutritional status assessment and be reviewed by a dietician as necessary. Many patients need definitive nutritional support, both pre- or post-treatment, via a NG (nasogastric) or RIG (radiologically-inserted gastrostomy) tube.
Curative Treatment
The mainstay of curative treatment for gastric adenocarcinoma is surgery. Patients who are fit enough should be offered peri-operative chemotherapy (typically 3 cycles of neoadjuvant and 3 cycles of adjuvant).
The aim of surgery is to achieve loco-regional control by removing the tumour and its local lymph nodes. The type of operation performed depends on the region of the malignancy:
- Proximal gastric cancers – total gastrectomy
- Distal gastric cancers (antrum or pylorus) – subtotal gastrectomy
The distal pancreas and spleen may be removed as well if there is direct invasion of these organs and still a chance of a curative resection
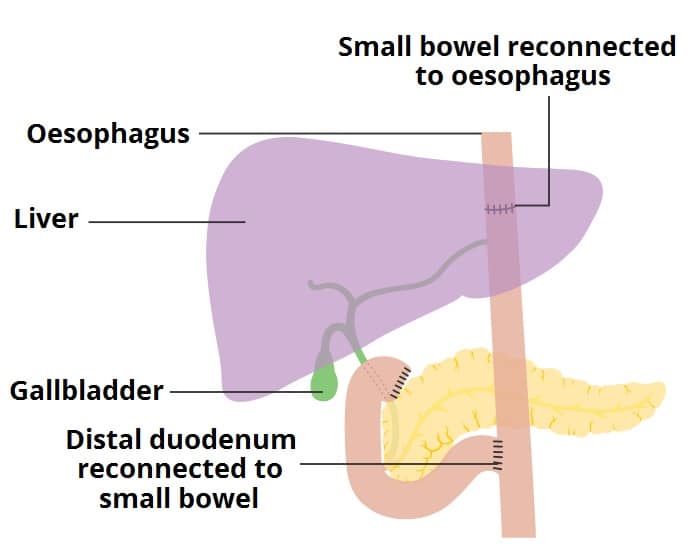
The most commonly used method in reconstructing the alimentary anatomy is the Roux-en-Y reconstruction as it gives the best functional result, in particular with less bile reflux. Post-gastrectomy, the distal oesophagus is end-to-end anastomosed directly to the small bowel, and the proximal small bowel is end-to-side anastomosed also to the small bowel (Fig. 4).
Patients with early T1a tumours (tumours confined to the muscularis mucosa) may be offered Endoscopic Mucosal Resection (EMR) or Endoscopic Submucosal Dissection (ESD). Current guidelines recommends these two options as standard treatment for differentiated adenocarcinoma without ulceration. They have the advantage of a greatly reduced morbidity, mortality, and quality of life impact, however will depend on the availability of expertise.
Gastrectomy Complications
A gastrectomy is a major operation. Mortality rates remain between 2-5% and quality of life remains poor for up to 6 months after surgery.
Specific complications include death (3-5%), anastomotic leak (5-10%), duodenal stump leak, re-operation, dumping syndrome, and vitamin B12 deficiency (patients need 3-monthly vitamin B12 injections).
Palliative Management
Unfortunately, most patients will be offered only a palliative approach due to the extent of disease at time of presentation. This may include chemotherapy, best supportive care, or stenting (for patients who have gastric outlet obstruction secondary to an obstructing cancer).
Palliative surgery (usually distal gastrectomy or bypass surgery (a gastro-jejunostomy)) can be used when stenting fails or is not available. It can also be used cautiously in the palliation of bleeding gastric tumours.
Complications
The main complications of gastric cancers are gastric outlet obstruction, iron-deficiency anaemia, perforation, and malnutrition.
The 10-year survival rate for stomach cancer overall is 15%, although this is stage-dependent. Most gastric cancers will present at an advanced stage with metastasis, which have a 5 year survival of <5%.
Key Points
- The main risk factors for gastric cancer include male gender, H. pylori infection, increasing age, and smoking
- The symptoms of gastric cancer are frequently vague and non-specific
- All suspected cases should undergo urgent OGD, and staging of gastric cancers should be done via CT chest-abdomen-pelvis and staging laparoscopy
- Curative treatment options for gastric cancers include total or subtotal gastrectomy with adjuvant and neo-adjuvant chemotherapy
- EMR and ESD can be considered for early stage cancers limited to the mucosa