Introduction
Dysphagia refers to difficulty in swallowing. Dysphagia occurs from any abnormal delay in the transit of liquids or solids during the oropharyngeal or oesophageal stages of swallowing, and can be either a transient delay or a fixed delay.
It is becoming an increasingly common presentation in more developed countries, largely due to an aging population. Causes of dysphagia can be categorised into mechanical obstruction (e.g. oesophageal cancer) or motility disorders (e.g. achalasia).
However, unless the history is convincing otherwise, any patient presenting with dysphagia should be assumed to have an upper gastrointestinal tract malignancy until proven otherwise. As such, patients presenting with dysphagia need an urgent upper GI endoscopy as first line investigation
In this article, we shall look at the causes, clinical assessment, and management of a patient with dysphagia.
Aetiology
The main causes of dysphagia can be divided into those resulting from a mechanical obstruction and those from a motility disorder:
- Mechanical
- Oesophageal cancer, Gastric cancer, or Head & Neck cancer
- Benign oesophageal strictures
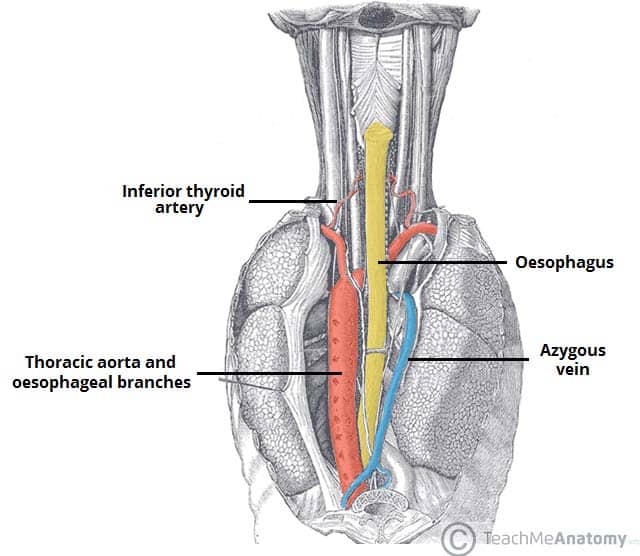
- Extrinsic compression (e.g. thyroid goitre)
- Pharyngeal pouch
- Foreign body (mainly in children)
- Oesophageal web (e.g. Plummer-Vinson syndrome, Fig 2)
- Motility
- Cerebrovascular accident
- Achalasia
- Diffuse oesophageal spasm
- Eosinophilic oesophagitis
- Neurological disorders, such as multiple sclerosis, amyotrophic lateral sclerosis, or myaesthenia gravis
- Muscular disorders, such as muscular dystrophy
- Rheumatological conditions, such as systemic sclerosis
Clinical Features
In the assessment of dysphagia, clarify the exact nature of the symptom, including duration and frequency*. Ensure to clarify further:
- Is there difficulty in initiating the swallowing action?
- Do you cough after swallowing?
- Do you have to swallow a few times to get the food to pass your throat?
*Difficulties in swallowing solids versus liquids is actually a poor differentiator between pharyngeal and oesophageal causes of dysphagia
Further symptoms to ask in addition to the dysphagia should include any reflux or dyspepsia, hoarse voice, or referred pain (to neck or ear). Patients will often have significant weight loss from dysphagia, due to not being able to consume sufficient calories.
Any dysphagia should be differentiated from odynophagia (pain when swallowing), as this may simply be due to a painful swallow, which itself has different causes.
On general examination, assess for any overt motor dysfunction, resting tremor, or dysarthria, that may point towards a more neuromuscular cause for the dysphagia.
Ensure to examine the mouth for any obvious oral disease (Fig. 3) and examine the neck for any lymphadenopathy. Examine the abdomen, specifically noting any abdominal masses palpable.
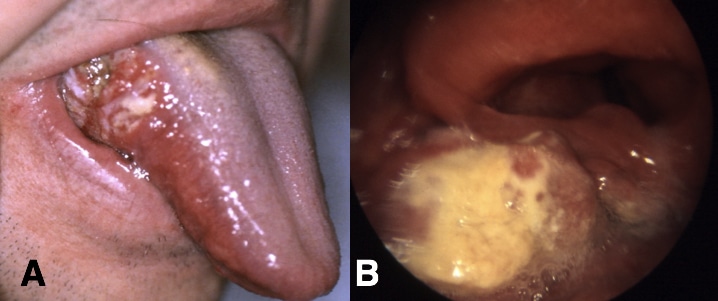
Figure 3 – Squamous Cell Carcinoma of the Head and Neck in the (A) Oral cavity and (B) Hypopharynx
Investigations
Any patient presenting with dysphagia should have routine bloods, including full blood count, liver function tests, and thyroid function tests, which can help aid in the diagnosis.
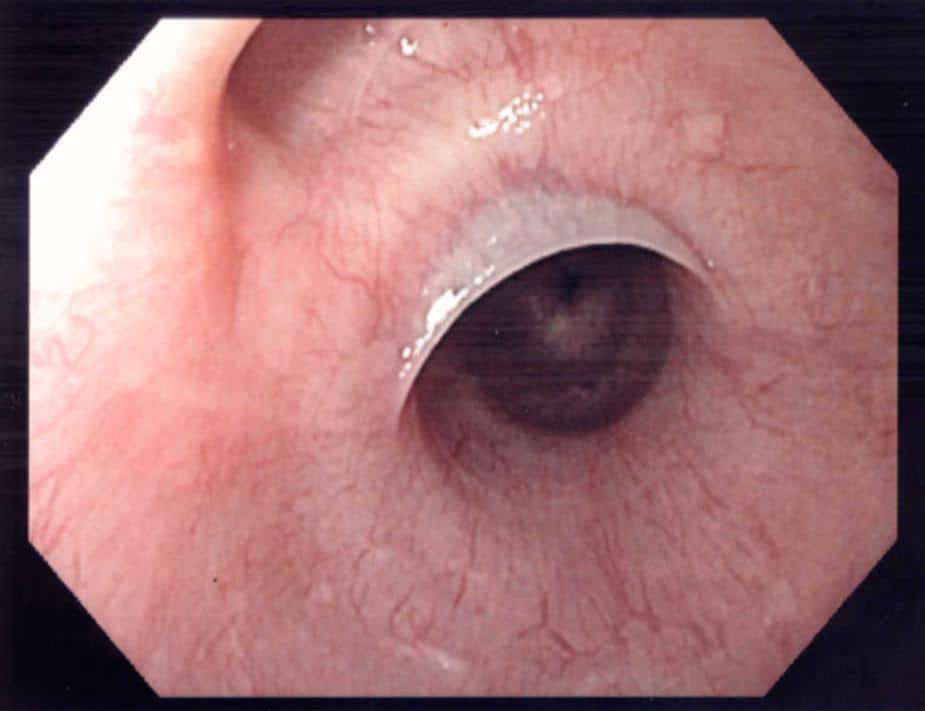
First line investigation for the majority of patients with dysphagia should upper GI endoscopy (OGD, Fig. 24. This will assess for any mechanical cause and importantly can exclude any upper GI malignancy*.
*Further management options may be performed via OGD in certain mechanical causes too (e.g. dilatation of benign oesophageal stricture)
Any further investigations will depend on the suspected underlying cause, however for cases where dysphagia persists despite a normal OGD (and no other obvious underlying cause is suspected), then a potential motility disorder should be investigated. Random oesophageal biopsies should be taken to investigate for eosinophilic oesophagitis.
In such cases, manometry testing is performed (Fig. 5), which assesses the motor function of the upper oesophageal sphincter (UES), the oesophageal body, and the lower oesophageal sphincter (LES). This can give a definitive diagnosis for certain motility disorders.
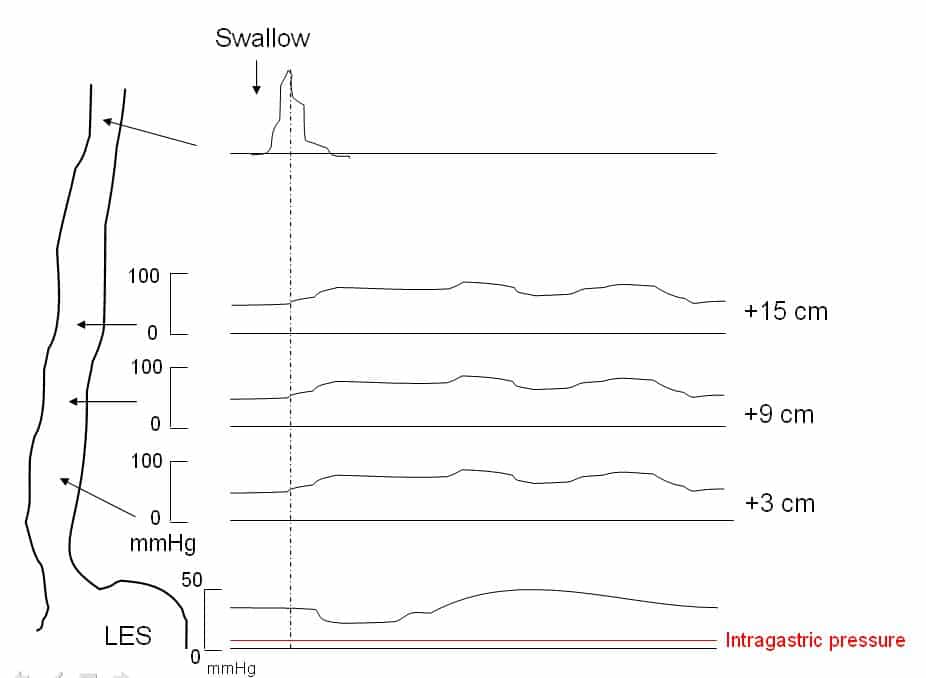
Figure 5 – Manometry results for a patient with achalasia
Management
The mainstay of management in dysphagia is treatment of the underlying cause.
Regardless of cause, patients with dysphagia are often significantly malnourished, therefore consideration of their nutritional status and involvement of a dietician is paramount. Moreover, patients with certain motility disorders causing dysphagia (e.g. following a stroke) will warrant referral to a Speech and Language Therapist.
Patients with dysphagia secondary to a cancer should be managed in the appropriate MDT meeting. For those with motility disorders, often medical management is trialled first, before either endoscopic or surgical intervention. Patients with neurological disorders causing dysphagia (e.g. Myasthenia Gravis) are best managed via a neurologist, or the relevant medical speciality necessary, to treat the underlying cause where possible.
Key Points
- Causes of dysphagia can be broadly categorised into mechanical obstruction or motility disorders
- Most cases of dysphagia should be investigated with an urgent upper GI endoscopy as first line
- Treatment depends on the underlying cause
- Ensure early involvement of dieticians, as nutritional status is often compromised