Introduction
Haematemesis is defined as vomiting fresh blood. This occurs as a result of bleeding occurring in any part of the upper gastrointestinal tract.
It has a wide range of causes and patients can present in a spectrum of illness severity. The management require depends on the underlying cause for the haematemesis.
In this article, we shall look at the causes, investigations, and management of haematemesis.
Differential Diagnosis
Oesophageal Varices
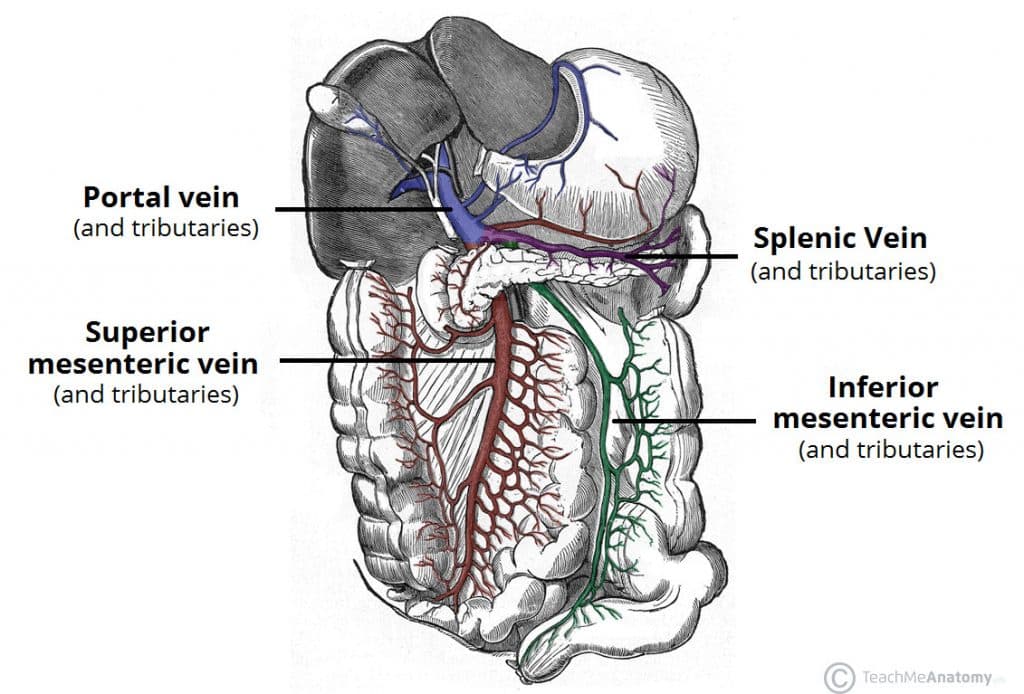
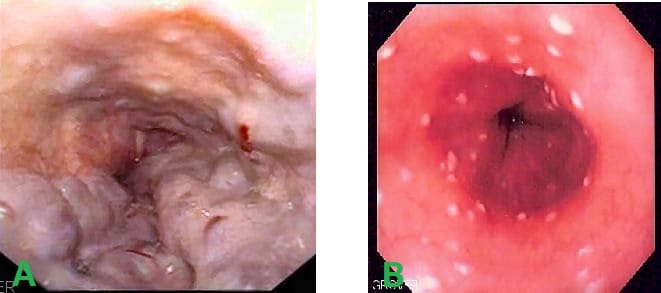
Oesophageal varices refer to dilations of the porto-systemic anastomoses in the oesophagus. They most commonly occur due to portal hypertension secondary to liver cirrhosis; the dilated veins are swollen and thin-walled, hence prone to rupture and the potential to cause a catastrophic haemorrhage (Fig 2A).
The most common underlying cause for oesophageal varices is alcoholic-related liver disease (ArLD), however can occur with any patient with chronic liver disease. Any haematemesis in a patient with a known chronic liver disease should be urgently investigated for potential variceal bleeding.
Peptic Ulcer Disease
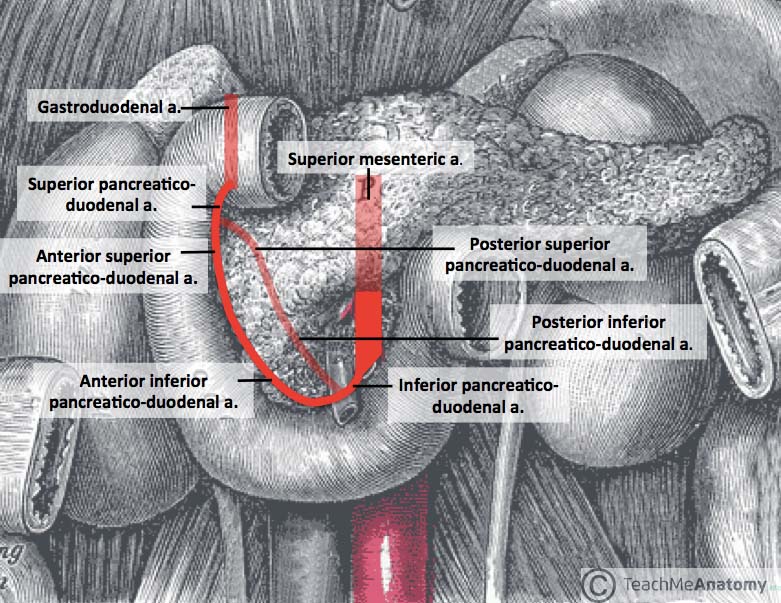
Peptic ulcer disease is responsible for about 60% of patients presenting with haematemesis. Peptic ulceration can result in erosion into the blood vessels supplying the upper GI tract (most commonly on the lesser curve of the stomach (20%) or posterior duodenum (40%)). which can result in significant haemorrhage.
Whilst it can affect any patient group, it should be especially suspected in those with known active peptic ulcer disease, a recent history of NSAID use or steroid use, or known H. pylori infection.
Mallory-Weiss Tear
A Mallory-Weiss tear is a relatively common phenomenon, typified by episodes of severe or recurrent vomiting, then followed by minor haematemesis. Such forceful vomiting causes a tear in the epithelial lining of the oesophagus, resulting in a small bleed.
Most cases are benign and will resolve spontaneously, therefore providing the patient reassurance and monitoring is usually all that is required.
Oesophagitis
Oesophagitis is a condition that describes inflammation of the intraluminal epithelial layer of the oesophagus, most often due to either reflux disease (GORD) or less commonly from infections (typically Candida Albicans, Fig 2B), medication (such as bisphosphonates), radiotherapy, ingestions of toxic substances, or Crohn’s disease.
Other Causes
Other less common causes of haematemesis include gastric cancer or oesophageal cancer, or vascular malformations (e.g. angiodysplasia).
Clinical Features
The key facts to ascertain from a history of haematemesis are:
- Features of haematemesis – timing, frequency, and the volume of bleeding
- Associated symptoms – including dyspepsia, dysphagia, melena, or weight loss
- Past medical history – including the smoking & alcohol status
- Drug history – use of steroids, NSAIDs, anticoagulants, or bisphosphonates
A full abdominal examination to assess for epigastric tenderness or peritonism, hepatomegaly, and for any stigmata of liver disease.
Investigations
Initial Investigations
All patients with suspected haematemesis should undergo routine blood tests, including FBC, U&Es, LFTs, and clotting, to help investigate for underlying causes and to stratify patient risk
Ensure all patients with haematemesis must have a Group and Save requested, and any haemodynamic instability should have blood urgently cross-matched too.
Further Investigations
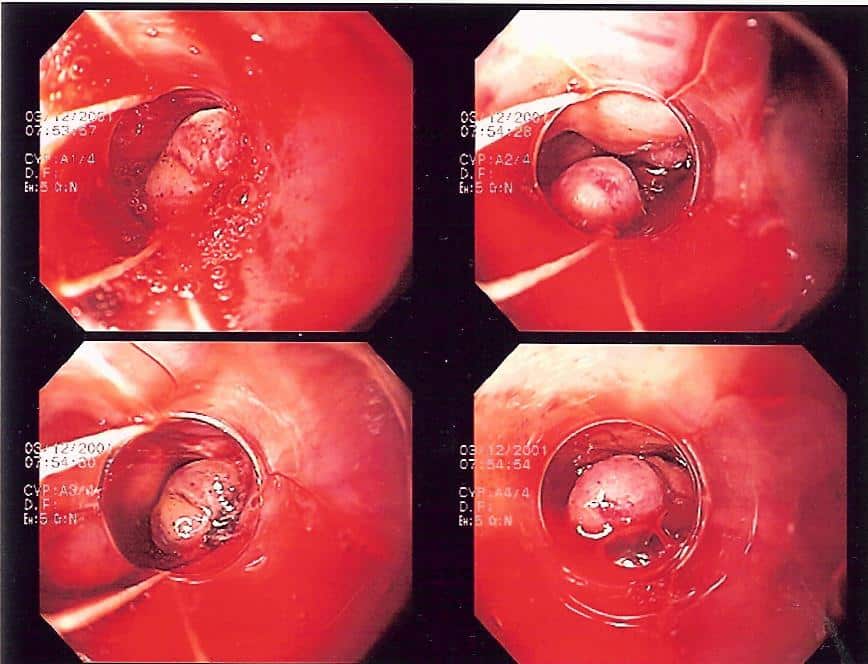
All patients with haematemesis must undergo a gastroscopy (OGD) for further assessment. This will not only potentially identify the cause of the bleeding, but also can perform definitive intervention in certain cases (e.g. banding of varices)
The urgency by which an OGD is performed should be determined by the patients Glasgow-Blatchford bleeding score (GBS), used to risk stratify patients based purely on clinical and biochemical parameters. After endoscopy, the Rockall score is used to predict mortality and rebleeding risk based on endoscopy findings.
Glasgow-Blatchford Bleeding Score
The Glasgow-Blatchford bleeding score (GBS) is a scoring system used to risk stratify patients admitted with an upper GI bleed, based purely on clinical and biochemical parameters. This allows for appropriate management of further investigations, especially as the score can be calculated prior to any gastroscopy.
Interpretation will vary across endoscopy departments, but scores ≥6 have been associated with a >50% risk of needing an intervention.
| 1 | 2 | 3 | 4 | 5 | 6 | |
| Urea (mmol/L) | 6.5-8.0 | 8.0-10.0 | 10.0-25.0 | >25 | ||
| Hb (g/L) | 12.0-12.9 | 10.0-11.9 | <10.0 | |||
| Systolic BP | 100-109 | 90-99 | <90 | |||
| Pulse (bpm) | >100 | |||||
| Melena | Present | |||||
| Syncope | Present | |||||
| Known Hepatic Failure | Present | |||||
| Cardiac Failure | Present |
Table 1 – Glasgow-Blatchford scoring criteria
In cases where the OGD is normal (or in certain scenarios where the patient cannot undergo endoscopic procedures), a CT angiogram can be performed if ongoing bleeding is suspected. Further embolisation of any active bleeding sites can then be considered if identified on angiogram*
*In peptic ulcer disease, most commonly the gastro-duodenal artery is the cause of active bleeding (Fig. 3), having been eroded into by a posterior D1 ulcer
Management
In any critically unwell patient, an A to E approach should be used to stabilise the patient before considering definitive management steps, as patients with haematemesis can be extremely unstable.
Any haemodynamically unstable patient with haematemesis should have large bore intravenous access obtained and urgent blood transfusion(s) given, for the patient to be stabilised (even if partially). Any deranged coagulation should be corrected as appropriate, which may include use of fresh frozen plasma (FFP) +/- platelets in patients with impaired liver function.
Most cases will warrant a gastroscopy, from which a range of therapeutic options are available depending on the underlying causes suspected or confirmed:
- Peptic ulcer disease – requires injections of adrenaline and cauterisation of the bleeding during endoscopy, then patients commenced on high dose intravenous proton pump inhibitor (PPI) therapy to reduce gastric acid secretion
- Oesophageal varices – management should be swift and performed at the same time as active resuscitation, including the use of blood products, prophylactic antibiotics, and somatostatin analogues (e.g. terlipressin or octreotide, to reduce splanchnic blood flow)
- Endoscopic banding is the most definitive method of management but can be technically difficult (Fig. 3); a Sengstaken-Blakemore tube can be used in severe or uncontrollable cases, inserted to the level of the varices and inflated to compress the bleeding as a temporary control
Surgical intervention is rarely required in upper GI bleeds, however may be considered in patients with ongoing GI bleeding with instability (or requiring continued transfusion), where endoscopic and interventional radiology treatments have failed. This often requires a laparotomy, therefore patient selection here is key. In the case of peptic ulcer bleeds, the bleeding vessel may then be underrun with a suture.
Key Points
- The majority of cases of haematemesis are caused by peptic ulcer disease
- All cases of haematemesis should be investigated with a gastroscopy
- The Glasgow-Blatchford bleeding score (GBS) can be used to risk stratify patients admitted with an upper GI bleed
- Ensure urgent resuscitation with blood products for patients presenting with haematemesis; definitive management will depend on the underlying cause