Introduction
Femoral hernias are a relatively uncommon hernia but are an important problem due to their high rate of strangulation from their narrow neck
Femoral hernias occur when abdominal viscera or omentum passes through the femoral ring and into the potential space of the femoral canal.
Femoral hernias account for approximately 5% of abdominal hernias and are more common in women than men (ratio 3:1), because of the wider anatomy of the female bony pelvis. It is very rare for femoral herniation to occur in a child.
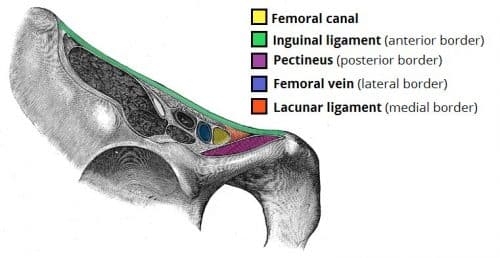
Femoral Canal Anatomy
The femoral canal (Fig. 1) is an anatomical compartment, located in the anterior thigh. It contains lymphatic vessels, lymph nodes and some loose connective tissue. The superior border of the femoral canal is the femoral ring, which is covered by the femoral septum (a connective tissue layer).
The rigidity of the borders of the femoral ring, especially the concave margin of the lacunar ligament and the bony pelvis posteriorly, results in femoral hernias being prone to obstruction and strangulation requiring urgent surgical intervention.
Risk Factors
The main risk factors for developing a femoral hernia include female gender, pregnancy (higher incidence in multiparous women), raised intra-abdominal pressure (e.g. heavy lifting, chronic constipation), and increasing age
Clinical Features
Femoral hernias will commonly present as a small lump in the groin. Whilst a femoral hernia is usually asymptomatic (aside from the lump) at presentation, due to the anatomy of the femoral canal, around 30% of femoral hernia cases will present as an emergency, either obstruction or strangulation.
When examining the groin, is important to identify the exact location of the lump in the groin in order to decide which type of hernia is present (although often, particularly in obese patients, it is not clear):
- Femoral hernia – found infero-lateral to the pubic tubercle (and medial to the femoral pulse)
- Inguinal hernia – found supero-medial to the pubic tubercle*
The tightness of the femoral ring means that the hernia is unlikely to be reducible. Ensure to check for overlying skin changes or tenderness, which can suggest complications from the hernia.
*A femoral hernia can roll up superiorly and in front of the inguinal ligament, therefore are often misdiagnosed as inguinal
Emergency Presentation of a Hernia
The complications that can occur with any hernia are:
- Irreducible / incarcerated – the contents of the hernia are unable to return to their original cavity
- Obstruction – the bowel lumen has become obstructed, leading to the clinical features of bowel obstruction
- Strangulation – compression of the hernia has compromised the blood supply, leading to the bowel becoming ischaemic
An abdominal wall hernia that has strangulated will present as an irreducible and tender lump, the pain often being out of proportion to clinical signs. A strangulated hernia is a surgical emergency and requires an urgent operation.
Differential Diagnosis
The differential diagnoses for a lump in the groin include an inguinal hernia, femoral canal lipoma, a lymph node, a saphena varix*, or a femoral artery aneurysm.
Athletic Pubalgia occurs following a small tear in rectus sheath through which impingement of abdominal wall musculature can occur, most often in young athletes.
*Saphena varix will disappear when lying flat, have palpable thrill when coughing, and there will be the presence of varicose veins elsewhere
Investigations
All patients presenting acutely to hospital with a groin lump should have routine blood tests performed, including a FBC, clotting screen, and Group & Screen. In cases of suspected strangulation, a venous blood gas will aid assessment
Whilst the diagnosis can be made clinically, additional imaging is often required; this can aid to delineate anatomy and assess for any underlying complication from the hernia (obstruction or strangulation):
- Ultrasound scan can confirm the presence of the femoral hernia (Fig. 2), yet these are often operator-dependent
- CT abdomen-pelvis scan with intravenous contrast can confirm the presence of a femoral hernia and can assess for radiological features of ischaemia and bowel obstruction
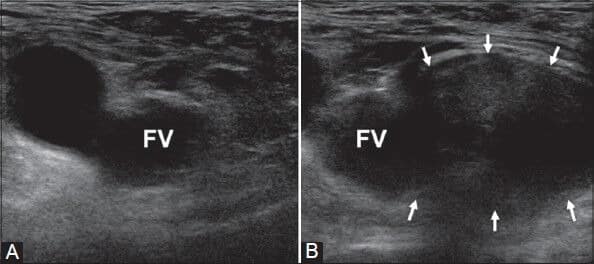
Figure 2 – Ultrasound image of a right femoral hernia, arising medial to the femoral vein (FV), assessed at rest (A) and during Valsalva (B)
Management
All femoral hernias should be managed surgically. For those presenting electively, these should be fixed ideally within 2 weeks of presentation, due to their high risk of strangulation.
The general principles of the operation involves reducing the hernia and then narrowing the femoral ring with sutures medially between the pectineal and inguinal ligaments or with a mesh plug. Care must be taken to avoid the femoral vein laterally.
In the elective setting, three different surgical approaches have been described for femoral hernias.
- Low approach (Lockwood) – the incision is made below the inguinal ligament, which has the advantage of not interfering with the inguinal structures but does result in limited space for access to the intraperitoneal space or the removal of any compromised small bowel
- High approach (McEvedy) – the incision is made above the inguinal ligament, allowing access to the preperitoneal and intraperitoneal space via the lateral edge of the rectus sheath; the main benefit of this approach is that the integrity of the posterior wall of the inguinal canal is not compromised
- This is the preferred technique in an emergency intervention due to the easy access to compromised small bowel for any resection if necessary
- Inguinal approach (Lotheissen) – the incision is similar to that for an open inguinal hernia repair, and the inguinal canal is entered via incising the external oblique aponeurosis; the preperitoneal and intraperitoneal space can then be accessed via incising the transversalis fascia
Most surgeons today perform modified versions of the three classically described approaches. Depending on availability and expertise, laparoscopic approach can also be used for diagnosis, assessment of bowel viability, and even laparoscopic repair.
Complications
The risk of strangulation of femoral hernias increases with time following initial diagnosis; after 3 months the risk of strangulation is 22% and reaches 45% after 21 months.
As with any hernia, there is also a risk of becoming obstructed, however femoral hernias containing small bowel are commonly Richter’s hernias, due to the small size of the hernia defect. therefore the clinical features of obstruction may not be present initially.

Figure 3 – Full circumference gangrenous segment of the small intestine caused by strangulation
Key Points
- Female gender and pregnancy increase the risk of developing a femoral hernia
- Femoral hernias commonly present as an emergency; any patient (particularly older females) presenting with vomiting must have their groins examined as it is commonly missed
- Femoral hernias have a high rate of strangulation, urgent surgery is therefore mandatory
- Surgical management can be taken via a low, inguinal or high approach, with laparoscopy being an option as well