Introduction
Gastroenteritis is the term used to describe inflammation of the gastrointestinal tract. It is usually considered to be infective in origin when the term is used, however it can describe non-infective causes too.
For infective cases, they are most often transient, presenting with combination of symptoms such as diarrhoea, vomiting, and abdominal pain, although not all have to be present in order to make the diagnosis. The most common aetiology is viral, contributing to 30-40% of gastroenteritis in more-developed countries.
Importantly, subtle differences in the length of time between ingestion of food and development of symptoms can often reveal the causative agent; as a general rule: bacterial toxins = hours, viruses = days, bacteria = weeks, parasites = months
Clarification of Terminology
- Diarrhoea: 3 or more loose stools or stools with increased liquid per day
- Acute diarrhoea: Lasting less than 14 days
- Chronic diarrhoea: Lasting more than 14 days
- Dysentery: Subtype of gastroenteritis characterised by loose stools with blood and mucus
- Travellers’ diarrhoea: More than 3 loose stools commencing within 24 hours of foreign travel, with or without cramps, nausea, fever, or vomiting
Risk Factors
The main risk factors for infective gastroenteritis include poor food preparation, especially in handling and cooking, immunocompromise, and poor personal hygiene
Clinical Features
Patients will typically present with a cramp-like abdominal pain and diarrhoea (with or without blood or mucus). There may be associated vomiting, night sweats, or weight loss reported.
On examination, the patient will often be dehydrated (of varying severity) with potential pyrexia.
Specific features from the history to note for any suspected cases of infective gastroenteritis include:
- Bowel movements(blood stained, mucus, profusely watery)
- Affected familyor friends
- Recent travel abroad
- Recent use of antibioticswithin the previous four weeks
- Can suggest potential difficileinfection (discussed below)
In rare cases, patients may present with specific complications of certain causative organisms, such as Guillain Barre syndrome, reactive arthritis, or haemolytic uraemic syndrome.
Investigations
Investigations are not necessary for most cases, as the condition is usually self-limiting.
Stool cultures may be warranted in cases with blood or mucus in the stool, if the patient is immunocompromised, or if severe or persistent.
Cross sectional imaging, such as a CT scan, may be helpful in severe acute cases to rule out other causes for the patients symptoms (e.g. diverticulitis)
Management
The general points of management for any patient with gastroenteritis include:
- Rehydration, encouraging oral fluid intake where possible
- If severe dehydration or unable to tolerate oral fluid, the patient may need admission for intravenous fluid rehydration
- Educationto prevent future episodes
- Exclusionfrom work is usually 48 hours from the last episode of vomiting or diarrhoea
In the UK, both food poisoning and infectious bloody diarrhoea are notifiable diseases and it is the duty of the diagnosing doctor to notify the appropriate Public Health body.
Certain organisms are also notifiable (e.g. Campylobacter and Salmonella in the UK), however this is the duty of the laboratory identifying the organism to notify the Public Health body about this.
Infective Causes
Viruses
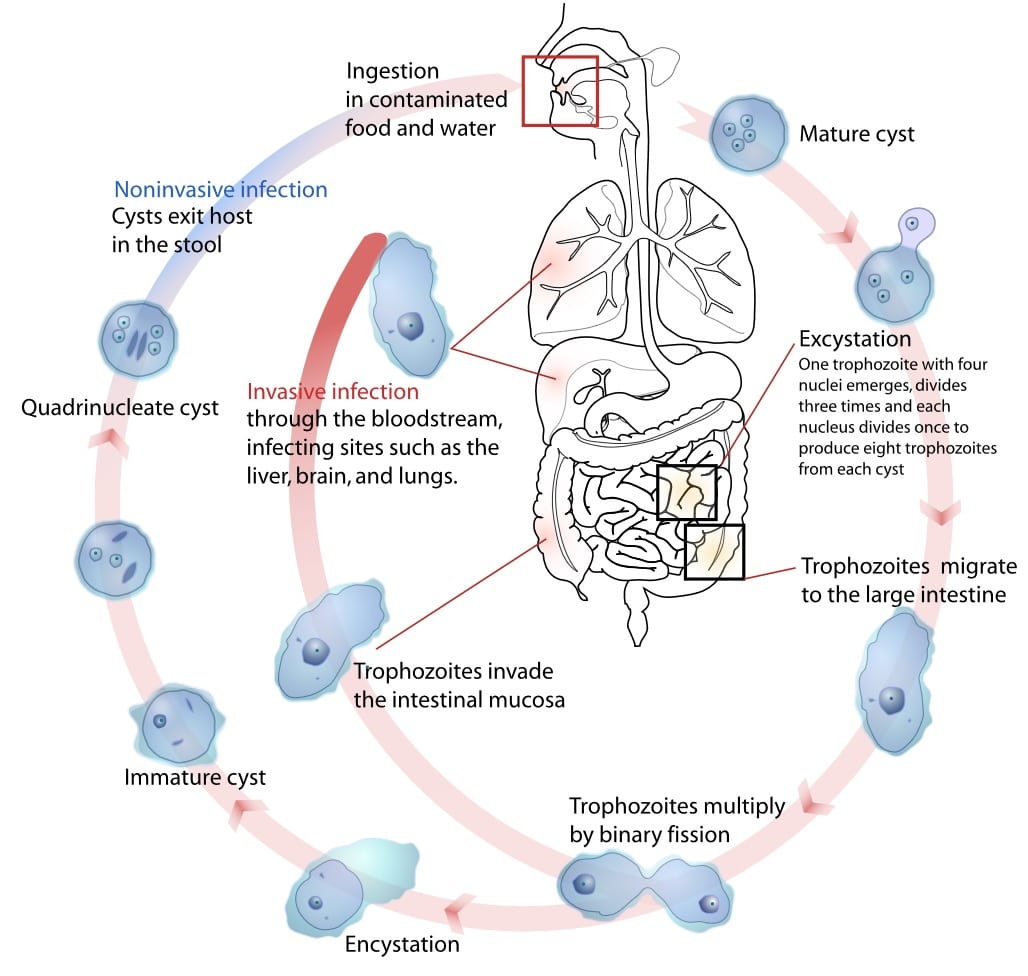
- Norovirus – single-stranded RNA virus (Fig. 1), the most common form of viral gastroenteritis in adults, presents with abdominal cramps, watery diarrhoea, and vomiting, usually lasting 1-3 days
- Rotavirus – double-stranded RNA virus, results in a severe diarrhoea among infants and young children, generally self-resolves in less than a week
- Adenovirus – double-stranded DNA virus, a common cause of diarrhoea in children
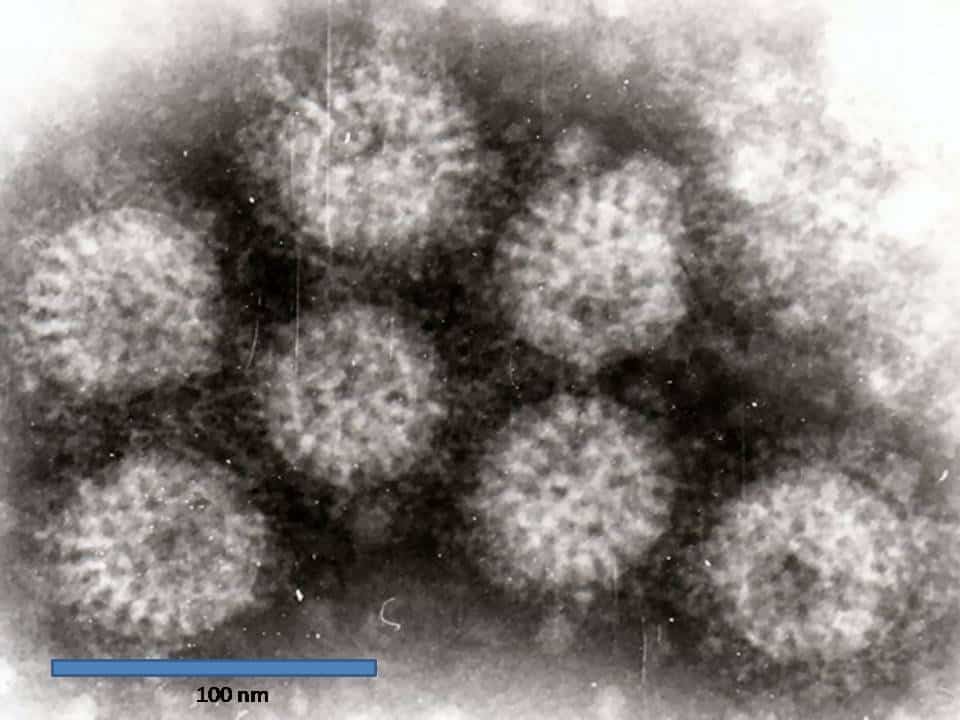
Figure 1 – Rotavirus particles, as seen on electron microscopy
Bacteria
- Campylobacter – Gram negative bacillus (Fig. 2), the most common cause of food poisoning (typically from ingestion of affected undercooked chicken, eggs, or milk), can have a prodrome of fatigue, fever, or myalgia, followed by nausea, abdominal cramps, and diarrhoea
- Campylobacter infections can also result in reactive arthritis, Guillan Barre syndrome, haemolytic uraemic syndrome, and thrombotic thrombocytopaenic purpura
- E. Coli – Gram negative bacillus, typically transmitted through contaminated foodstuffs (but can also spread from animals to human or from person to person contact); several forms of the bacteria exist, but Enterotoxigenic E. coli (ETEC) is the most common cause of Travellers’ diarrhoea
- coli serotype 0157:H7 is associated with haemorragic uraemic syndrome
- Salmonella – Gram negative flagellated bacillus (two serotypes most commonly associated with gastroenteritis, S. typhimurium and S. enteritidis), transmitted through undercooked poultry or raw eggs; results in fever, vomiting, abdominal cramps, and bloody diarrhoea
- Shigella – Gram negative bacillus, commonly acquired from contaminated dairy products and water; presents with fever, abdominal pain, or bloody diarrhoea

Figure 2 – Electron microscopy of Campylobacter jejuni, showing its characteristic spiral shape
Bacterial Toxins
Toxins from bacteria often cause an acute onset of diarrhoea and vomiting and symptoms tend to last less than 24 hours. Common bacterial toxins can arise from:
- Staphylococcus aureus – typically found in meat or dairy products, even re-heating of the cooked food does not destroy the exotoxin (even if the bacteria are destroyed)
- Bacillus cereus – usually found in reheated rice, known to cause rapid-onset vomiting and abdominal cramps
- Clostridium perfringes – typically acquired from re-heating meat dishes, predominantly causes diarrhoea
- Vibrio cholera – acquired most commonly from contaminated water supplies and causes profound watery painless diarrhoea (an oral vaccine is available)
Parasites
In any patient with Travellers’ diarrhoea, parasites are more likely to be the causative organism
- Cryptosporidium – protozoan that typically causes a self-limiting watery diarrhoea and abdominal cramps, however can be life-threatening in those who are immunocompromised; diagnosis is made with stool culture for ova, cysts, and parasites.
- Entamoeba histolytica – anaerobic amoebozoan that becomes acquired from the ingestion of food or water contaminated with faeces (Fig. 3), presents with bloody diarrhoea, abdominal pain, and fever (can also result in liver abscess); stool culture for ova, cysts and parasites is required for diagnosis, recommended treatment is metronidazole or tinidazole
- Giardia intestinalis – parasite transmitted through direct contact or faeco-oral route, can cause either acute disease (diarrhoea, fever, fatigue, nausea, and bloating) or chronic disease (steatorrhoea, malabsorption, and weight loss); diagnosis made with stool culture for ova, cysts and parasites, recommended treatment is metronidazole or tinidazole
- Schistosoma – also known as bilharzia, a fluke acquired through contaminated water, with acute schistosomiasis developing about a month after the initial infection, presenting with fever, malaise, abdominal pain, bloody diarrhoea, and severe cases even leading to chronic liver disease; eosinophilia may be seen on full blood count and a stool culture for ova, cysts and parasites is required, with treatment via praziquantel
Hospital-Acquired Gastroenteritis
The main pathogen for hospital-acquired gastroenteritis is C. difficile, a Gram positive organism that can develop following the use of broad-spectrum antibiotics, disrupting the normal microbiota of the bowel. This allows the excess overgrowth of the C. difficile bacteria, leading to the organism being able to also produce large amounts of exotoxins A & B
The exotoxins produce a sizeable immune response from the bowel, resulting in inflammatory exudate on the colonic mucosa (with intervening areas of normal mucosa), also known as pseudomembranous colitis. This presents clinically with severe bloody diarrhoea, and has the potential to develop into toxic megacolon (severely dilated bowel with high risk of perforation, Fig. 4) if left untreated. In severe cases, surgical intervention may be required.
Investigation requires both stool culture and C. difficile Toxin (CDT) testing*. First-line antibiotic for a first episode of C. difficile infection is oral vancomycin, however can be escalated to Fidaxomicin if ineffective.
*Results may report the presence of the bacteria but not of the toxin, in such cases these reports should be interpreted relative to the clinical picture
Non-Infective Causes
Non-infective causes of gastroenteritis include:
- Radiation colitis – inflammation of the gastrointestinal tract secondary to previous radiation therapy (often seen in those following radiotherapy for prostate cancer)
- Inflammatory bowel disease, such as Crohn’s Disease or Ulcerative Colitis
- Microscopic colitis – a condition where the colon is macroscopically normal on endoscopy, however biopsy demonstrates an increase in the number of inflammatory cells present
- Chronic ischaemic colitis– caused by a compromise in blood supply to the colon, most commonly affecting the watershed area around the splenic flexure, from chronic ischaemia
Key Points
- Gastroenteritis is caused by a variety of organisms, including viruses, bacteria, bacterial toxins, and parasites
- Important causes of dysentery include campylobacter, shigella, salmonella, and norovirus
- If the patient has travelled abroad, ensure to consider parasites in the differentials
- Have a low threshold for treatment in immunocompromised patients