Introduction
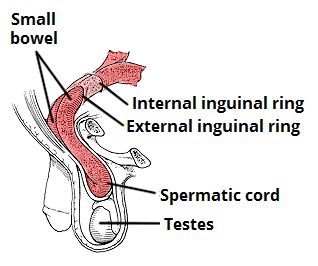
An inguinal hernia occurs when abdominal cavity contents enter the inguinal canal.
They are the most common type of hernia and account for around 75% of all anterior abdominal wall hernias, with a prevalence of 4% in those over 45 years.
In this article, we shall look at the classification, clinical features and management of inguinal hernia.
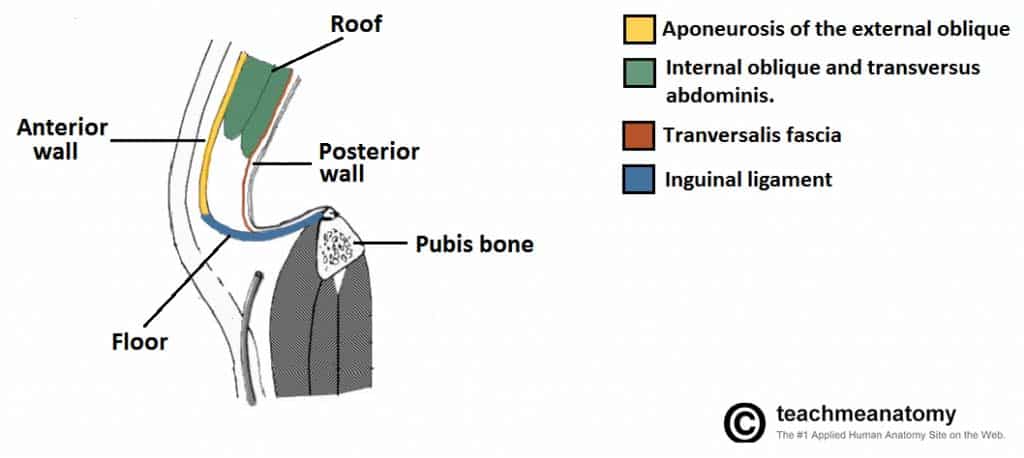
Figure 1 – Sagittal view of the inguinal canal, showing the borders
Classification
A hernia is defined as the protrusion of part or whole of an organ or tissue through the wall of the cavity that normally contains it. Inguinal herniae involve abdominal contents passing into the inguinal canal (and can continue into the scrotum)
The two main subtypes that can occur:
- Direct inguinal hernia (20%) – Bowel enters the inguinal canal “directly” through a weakness in the posterior wall of the canal, termed Hesselbach’s triangle*
- They occur more commonly in older patients, often secondary to abdominal wall laxity or a significant increase in intra-abdominal pressure
- Indirect inguinal hernia (80%) – Bowel enters the inguinal canal via the deep inguinal ring
- In younger patients, they arise from incomplete closure of the processus vaginalis, an outpouching of peritoneum allowing for embryonic testicular descent, therefore are usually deemed congenital in origin
These two types of inguinal hernia can only be reliably differentiated at the time of surgery by identifying the inferior epigastric vessels – indirect hernias will be lateral to the vessels whilst direct hernias will be medial to the vessels. In paediatric cases, they are nearly always indirect inguinal hernias
*Hesselbach’s triangle is bordered medially by the lateral border of the rectus abdominis muscle, superiorly by the inferior epigastric vessels, and inferiorly by the inguinal ligament
Risk Factors
The main factors that increase the risk of developing an inguinal hernia:
- Male gender
- Increasing age
- Raised intra-abdominal pressure, from chronic cough, heavy lifting, or chronic constipation
- High BMI
Clinical Features
The most common presenting symptom is a lump in the groin, which (for reducible herniae) will initially disappear with minimal pressure or when the patient lies down. There may be mild to moderate discomfort, which can worsen with activity or standing.
If the hernia becomes incarcerated, it can become painful and the lump cannot be reduced. The patient may also present with clinical features of bowel obstruction if the bowel lumen becomes blocked, or with features of strangulation* if the blood supply becomes compromised.
When examining any groin lump, specific features to note for any suspected inguinal hernia include:
- Cough impulse – remember that an irreducible hernia may not have a cough impulse
- Location – inguinal herniae appear superomedial to the pubic tubercle* (whilst femoral herniae appear inferolateral to the pubic tubercle)
- Reducible – On lying down or with gentle pressure
- If it enters the scrotum, can you get above it / is it separate from the testis
*This is not always clear on examination, especially if large and tender
Differentiation of Inguinal Hernia
Theoretically, to differentiate a direct from an indirect inguinal hernia, the examiner must reduce the hernia and then place pressure over the deep inguinal ring (located at the mid-point of the inguinal ligament), before asking the patient to cough.
If the hernia protrudes despite occlusion of the deep inguinal ring, this indicates a direct hernia, whereas if the hernia does not protrude, this indicates an indirect hernia.
This assessment is often seen as unreliable and the only definite method to differentiate them is at the time of surgery.
Differential Diagnosis
There are several differential diagnoses for a lump in the groin. These include femoral hernia, saphena varix, inguinal lymphadenopathy, lipoma, or groin abscess. If the mass extends into the scrotum, consider a hydrocoele, varicocoele, or a testicular malignancy.
Investigations
A hernia is typically a clinical diagnosis. Current Royal College of Surgeons Guidelines state that imaging should only be considered in patients if there is diagnostic uncertainty or to exclude other pathology.
If necessary, an ultrasound scan is recommended as first line imaging in the outpatient setting (Fig. 4). For patients with features of obstruction or strangulation, CT imaging will be required.
Management
Any patient with a symptomatic inguinal hernia (significant mass or discomfort) should be offered surgical intervention (see below).
The risk of strangulation is no more than about 2% per year with an inguinal hernia. Any patients presenting with evidence of strangulation (such as pain out of proportion to clinical features or deranged biochemical results) nearly always require urgent surgical exploration.
A third of patients with an inguinal hernia will never experience any symptoms (especially those identified incidentally on imaging). Discussions should take place around the likelihood of future surgical intervention and the symptoms of potential strangulation.
Emergency Presentation of a Hernia
The complications that can occur with any hernia are:
- Irreducible / incarcerated – the contents of the hernia are unable to return to their original cavity
- Obstruction – the bowel lumen has become obstructed, leading to the clinical features of bowel obstruction
- Strangulation – compression of the hernia has compromised the blood supply, leading to the bowel becoming ischaemic
An abdominal wall hernia that has strangulated will present as an irreducible and tender lump, the pain often being out of proportion to clinical signs. A strangulated hernia is a surgical emergency and requires an urgent operation.
Surgical Intervention
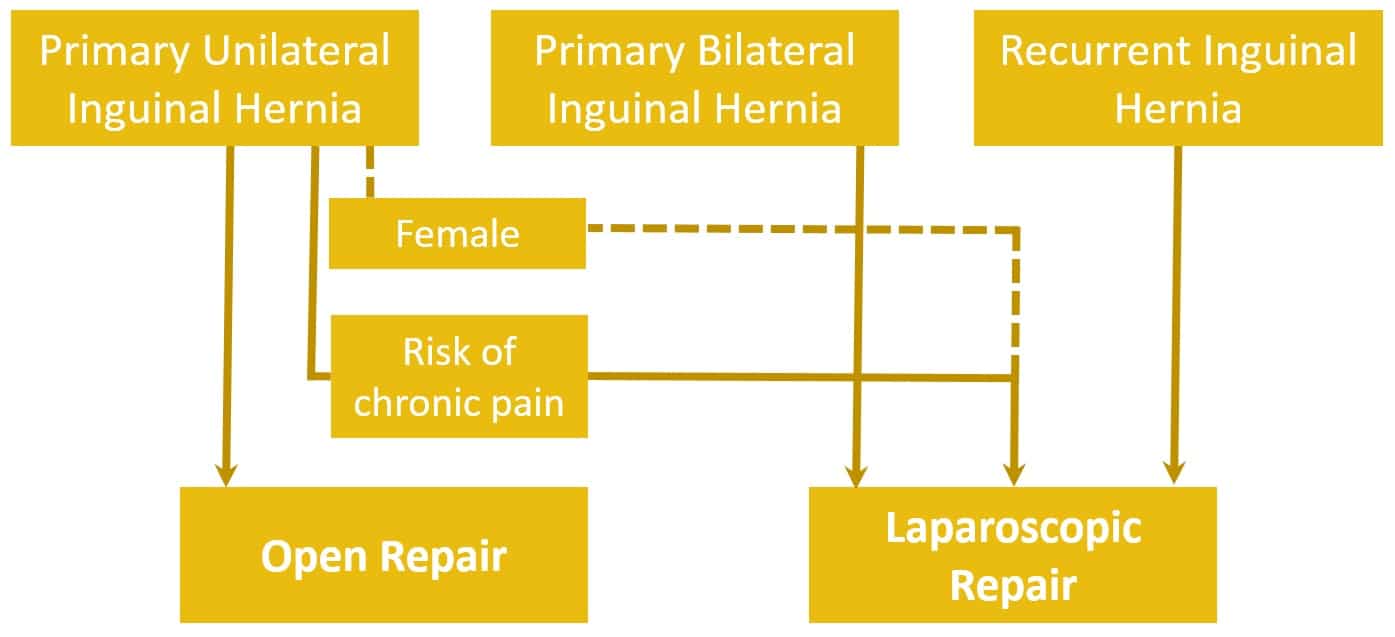
Hernia repairs can be performed via open repair or laparoscopic repair*; laparoscopic repairs are associated with longer operating times but quicker post-operative recovery, fewer complications, and less post-operative pain:
- Open mesh repairs are preferred for those with primary inguinal hernias and are deemed the most cost-effective technique in this patient group; they can be performed under general, spinal or local anaesthesia, dependent on patient fitness and surgeon preference
- Lichtenstein technique (with a mesh) is the most commonly technique used, whilst repair options without mesh include the Bassini or Shouldice methods
- Laparoscopic mesh repairs are preferred in those with bilateral or recurrent inguinal hernias; they can also be considered in certain patients with a primary unilateral hernia, mainly those at a high risk of chronic pain (young and active, previous chronic pain, or with a predominant symptom of pain) or in females (due to the increased risk of the presence of a femoral hernia)
- The two main types of laparoscopic repair are total extraperitoneal (TEP) or transabdominal pre-peritoneal (TAPP) repair
*A TAPP repairs involves establishing pneumoperitoneum, before accessing the preperitoneal space by incising the parietal peritoneum from the inside, whilst a TEP repair involves the entire operation being carried out within the preperitoneal space, without entering the peritoneal cavity, and a balloon dissector is used to expand and create room
Complications
The main complications of an inguinal hernia are incarceration, strangulation, and obstruction.
Potential complications following elective inguinal hernia repair include haemoatoma or seroma formation, recurrence (around 1% by 5years), chronic pain, or damage to vas deferens or testicular vessels (leading to ischaemic orchitis, and potentially sub-fertility)
Key Points
- An inguinal hernia can be classified as direct or indirect
- The diagnosis is a clinical one and only warrants further investigation if there is diagnostic uncertainty or features of complication
- Most cases are repaired via open approach