Introduction
Chronic pancreatitis is a chronic fibro-inflammatory disease of the pancreas, resulting in progressive and irreversible damage to the pancreatic parenchyma.
The incidence of chronic pancreatitis is quoted between 2-10 new cases per 100,000 people per year in Western countries. It has a male to female ratio of 4:1 and an average age of onset of 40 years.
The vast majority of patients present with chronic abdominal pain, however may also develop malabsorption, diabetes mellitus, and local complications during the course of the disease
Aetiology
The main causes of chronic pancreatitis are either chronic alcohol abuse (60%) and idiopathic (30%).
Less common causes include metabolic (hyperlipidaemia, hypercalcaemia), infection (both viral (e.g. HIV, mumps, coxsackie) and bacterial (e.g. Echinococcus), hereditary (e.g. cystic fibrosis), autoimmune (e.g. autoimmune pancreatitis (AIP) or SLE), anatomical (malignancy or stricture formation), or congenital anomalies (e.g. Pancreas divisum or Annular pancreas).
Clinical Features
The major symptom in chronic pancreatitis is chronic pain, which may be complicated by recurring attacks of acute pancreatitis (often termed “acute-on-chronic” pancreatitis). The pain is typically in the epigastrium and back, often associated with nausea and vomiting.
Due to the damage that has occurred to the pancreatic parenchyma, patients may also present with:
- Endocrine insufficiency – secondary to damage to the endocrine tissue of the pancreatic gland (islets of Langerhans), there is subsequent failure to produce insulin, resulting in impaired glucose regulation or eventual diabetes mellitus*
- Exocrine insufficiency – secondary to damage to the acinar cells, resulting in failure to produce digestive enzymes, causing malabsorption, presenting with weight loss, diarrhoea, or steatorrhoea
On examination, the abdomen will be soft, however the patient may be tender in the epigastrium. There is often evidence of significant cachexia.
Often concurrent pseudocysts are present, due to previous recurrent attacks of acute pancreatitis. Patients with pseudocysts may present with symptoms of mass effect, such as biliary obstruction or gastric outlet obstruction.
*Type 3c (pancreatogenic) diabetes is the term given to diabetes mellitus secondary to pancreatic disease resulting in endocrine dysfunction.
Differential Diagnosis
Differentials for patients with persistent central abdominal pain include peptic ulcer disease, reflux disease, abdominal aortic aneurysm, biliary colic, or chronic mesenteric ischaemia.
Investigations
Most patients presenting with abdominal pain should have a urine dip and routine bloods, including FBC and CRP. Serum amylase or lipase levels are often not raised in established disease.
In suspected cases of chronic pancreatitis, ensure to also check blood glucose (secondary to endocrine dysfunction) and LFTs (to ensure no concurrent obstructive jaundice)
A faecal elastase level will be low in most cases of chronic pancreatitis with exocrine insufficiency, often can aid the diagnosis.*
*The elastase enzyme is produced by the pancreas, being excreted into the bowel to aid with digestion, and importantly does not undergo any significant degradation during intestinal transit; as such, any exocrine dysfunction in chronic pancreatitis will present with low faecal elastase levels
Imaging
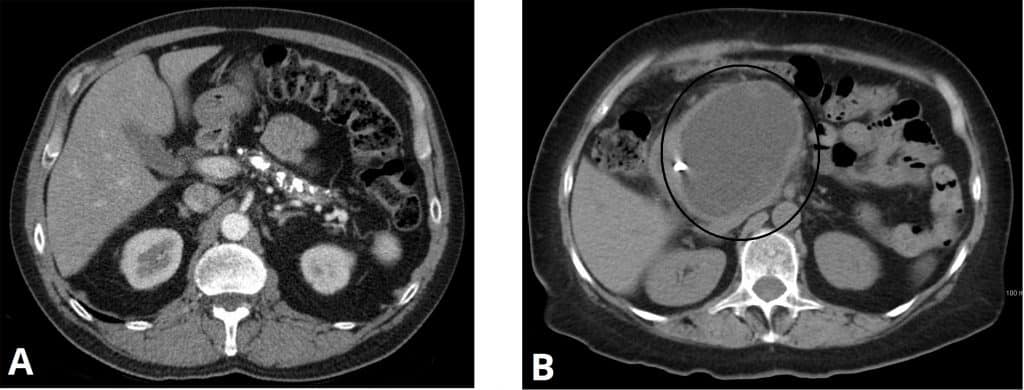
CT imaging can often show pancreatic atrophy or calcification, as well as any pseudocysts present (Fig. 2). Any overt causes for chronic pancreatitis, such as malignancy or congenital anomalies, may also be seen
The anatomy of the pancreas and the biliary tree can be determined using both ultrasound imaging or MRI imaging (specifically MRCP). However, a normal appearance of the pancreas on imaging does not necessarily exclude chronic pancreatitis.
Additional specialist tests, such as the secretin stimulation test or endoscopic ultrasound (EUS), may also be employed in cases of diagnostic uncertainty.
Management
Chronic pancreatitis can only be managed definitively by treating any reversible underlying cause. This can include alcohol cessation or statin therapy for hyperlipidaemia. However, analgesia becomes the mainstay of management for most cases of chronic pancreatitis.
Analgesic Approaches in Chronic Pancreatitis
The WHO analgesic ladder should be followed in acute flares of pain in patients with chronic pancreatitis. However, opioid analgesia for long-term pain is suboptimal and often associated with multiple side-effects. Instead, neuropathic analgesia, such as pregabalin, are deemed more effective in patients with chronic pancreatitis.
Non-pharmacological approaches include endosonography-guided celiac plexus blockade or thoracoscopic splanchnicectomy. Whilst they provide short-term pain relief, unfortunately they often have disappointing long-term effects.
Patients with malabsorption secondary to exocrine dysfunction may benefit from enzyme replacement (including lipases), such as Creon®, that can be taken with meals to good effect. Patients are also at risk of becoming deficient in fat-soluble vitamins (A, D, E and K), therefore ensure adequate vitamin supplementation and check bone density routinely.
Those with pancreatogenic diabetes may benefit insulin regimes, along with annual surveillance with HbA1c. Steroids are effective at reducing symptoms in chronic pancreatitis with an autoimmune aetiology only.
Non-Surgical Options
Endoscopic management is performed only in a select few patients where there is a targetable underlying cause.
Endoscopic retrograde cholangiopancreatography (ERCP) can be used for diagnostic and therapeutic purposes, including stone removal, stent placement, or sphincterotomy (especially in large duct pancreatitis).
Extracorporeal shock wave lithotripsy (ESWL) can be trialled in select cases, especially in those with large intraductal stones
Surgical Management
In those with large ductal stones, a Frey’s procedure may be performed, which involves coring out of the diseased part of the pancreatic head and formation of a lateral pancreaticojejunostomy; this allows better drainage of the main pancreatic duct into the jejunum
Those with pancreatic head disease but without ductal stones may benefit from a lateral pancreaticojejunostomy alone. If there is any suspicion of a pancreatic head malignancy, a pancreaticoduodenectomy (Whipples procedure) may be required.
There are limited surgical options available for those with chronic pancreatitis and small duct disease or diffuse sclerosis
Prognosis
Chronic pancreatitis is associated with significant morbidity and reduced quality of life, as it can be a challenging condition to manage effectively.
In some patients, the disease may eventually ‘burn out’ after many years of pain, leaving residual endocrine and exocrine insufficiencies.
Pancreatic malignancy is a risk in those who have had the disease for 20 years or more; new or evolving symptoms should therefore undergo investigation.
Key Points
- Chronic pancreatitis is caused by chronic alcohol excess in most cases
- Patients present with constant central abdominal and back pain, along with features of endocrine and exocrine insufficiency
- Reduced faecal elastase and CT imaging can be used to confirm the diagnosis
- Management is mainly based around symptom control, optimising analgesia, and nutritional support