Introduction
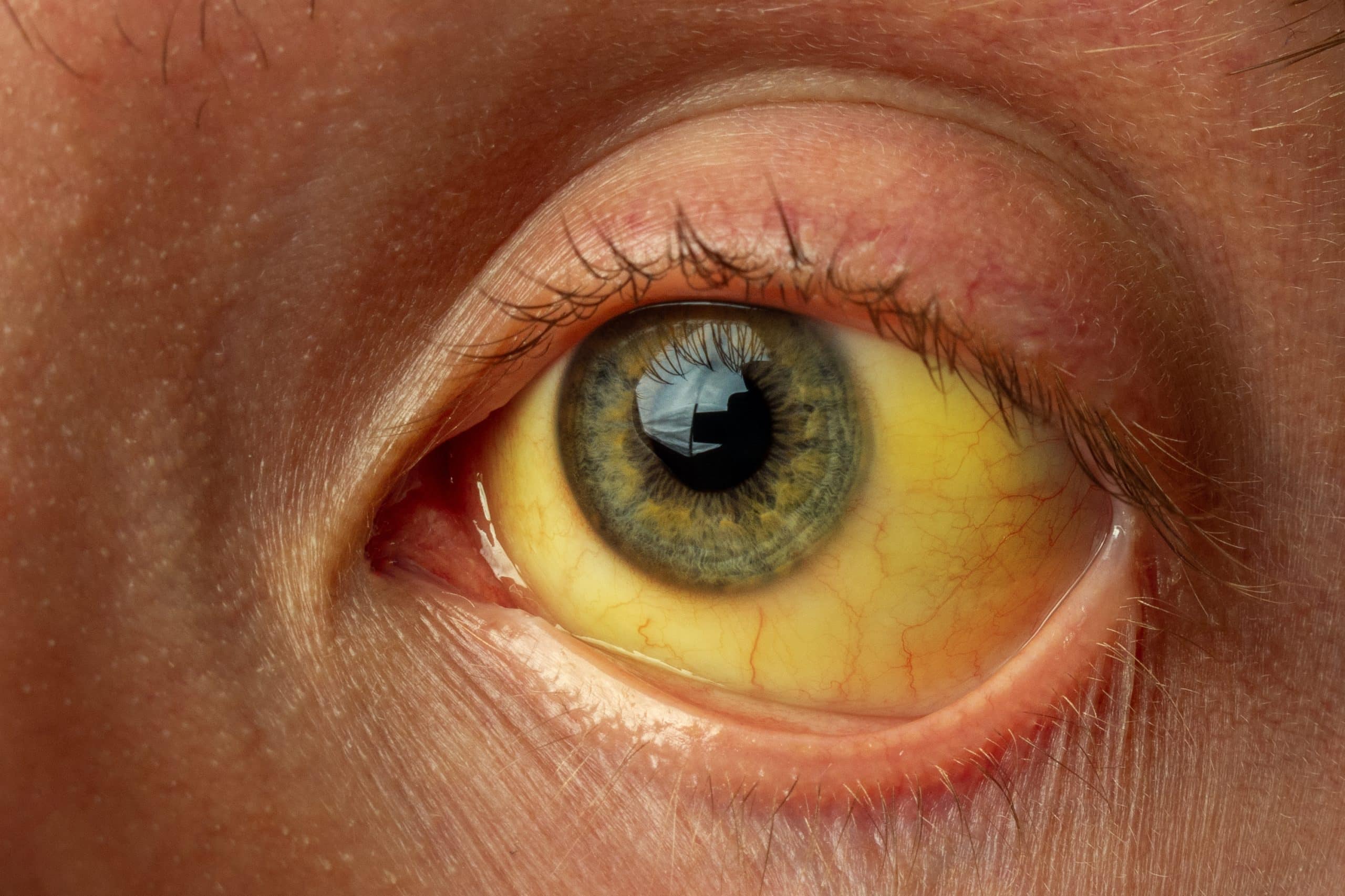
Jaundice refers to the yellow discolouration of the sclera and skin (Fig. 1) that is due to hyperbilirubinaemia, occurring at bilirubin levels roughly greater than 50 µmol/L.
Pathophysiology
Jaundice results from high levels of bilirubin in the blood. Bilirubin is the normal breakdown product from the catabolism of haem, and thus is formed from the destruction of red blood cells.
Under normal circumstances, bilirubin undergoes conjugation within the liver, making it water-soluble. It is then excreted via the bile into the gastrointestinal tract to be metabolised into urobilinogen, the majority of which is then egested in the faeces as stercobilin (the metabolic breakdown product of urobilingoen). Around 10% of urobilinogen is reabsorbed into the bloodstream and excreted through the kidneys. Jaundice occurs when this pathway is disrupted.

Figure 2 – Bilirubin is produced as a byproduct of haem metabolism
Types of Jaundice
There are three main types of jaundice: pre-hepatic, hepatocellular, and post-hepatic.
Pre-Hepatic
In pre-hepatic jaundice, there is excessive red cell breakdown which overwhelms the liver’s ability to conjugate bilirubin. This causes an unconjugated hyperbilirubinaemia.
Any bilirubin that manages to become conjugated will be excreted normally, yet it is the unconjugated bilirubin that remains in the blood stream to cause the jaundice.
Hepatocellular
In hepatocellular (or intrahepatic) jaundice, there is dysfunction of the hepatic cells. The liver loses the ability to conjugate bilirubin, but in cases where it also may become cirrhotic, it compresses the intra-hepatic portions of the biliary tree to cause a degree of obstruction.
This leads to both unconjugated and conjugated bilirubin in the blood, termed a ‘mixed picture’.
Post-Hepatic
Post-hepatic jaundice refers to obstruction of biliary drainage. The bilirubin that is not excreted will have been conjugated by the liver, hence the result is a conjugated hyperbilirubinaemia.
| Pre-Hepatic | Hepatocellular | Post-Hepatic |
|
|
|
Table 1 – Potential Causes for Jaundice, divided into pre-hepatic, hepatocellular, and post-hepatic
Bilirubinuria
A good estimation of which type of jaundice is present (prior to any further investigation) can be made from observing the colour of the urine.
Conjugated bilirubin can be excreted via the urine (as it is water soluble), whereas unconjugated cannot. Consequently, dark (‘coca-cola’) urine manifests in conjugated or mixed hyperbilirubinaemias, whereas normal urine is seen in unconjugated disease.
Moreover, those with an obstructive picture will likely note pale stools, due to the reduced levels of stercobilin entering the GI tract, which normally colours the stool.
Investigations
In many cases, the likely underlying cause can be elicited from the history, with the investigations simply confirming suspicions. Hence, whilst a complete list of investigations is given below, these should be tailored to the clinical features of the patient.
Laboratory Tests
Any patient presenting with jaundice should have the following bloods taken:
- Liver function tests (LFTs), as summarised in Table 2
- Coagulation studies (PT can be used as a marker of liver synthesis function)
- FBC (anaemia, raised MCV, and thrombocytopenia all seen in liver disease) and U&Es
- Specialist blood tests, as summarised below as part of a liver screen
| Blood Marker | Significance |
| Bilirubin | Quantify degree of any suspected jaundice |
| Albumin | Marker of liver synthesising function |
| AST and ALT | Markers of hepatocellular injury* |
| Alkaline Phosphatase | Raised in biliary obstruction (as well as bone disease, during pregnancy, and certain malignancies) |
| Gamma-GT | More specific for biliary obstruction than ALP (however not routinely performed) |
Table 2 – LFT serum markers. *as an estimate, if the AST:ALT ratio >2, this is likely alcoholic liver disease, whilst if AST:ALT is around 1, then likely viral hepatitis as the cause
Liver Screen
A liver screen can be performed for patients whereby there is no initial cause for liver dysfunction, tailored to whether acute or chronic liver failure
|
Viral Serology |
Non-Infective Markers |
|
| Acute Liver Injury |
|
|
| Chronic Liver Injury |
|
|
Table 3 – Acute and Chronic Liver Screens *Autoantibodies include anti-mitochondrial antibody (AMA), anti-smooth-muscle antibody (Anti-SMA), and anti-nuclear antibody (ANA), used to identify a variety of autoimmune liver conditions, such as primary sclerosing cholangitis (PSC)
Imaging
The imaging used will depend on the presumed aetiology. An ultrasound abdomen is usually first line, identifying any obstructive pathology present or gross liver pathology (albeit often user dependent).
Magnetic Resonance Cholangiopancreatography (MRCP) is used to visual the biliary tree, typically performed if the jaundice is obstructive, but US abdomen was inconclusive or limited, or as further work-up for surgical intervention.
A liver biopsy can be performed when the diagnosis has not been made despite the above investigations.
Management
The definitive treatment of jaundice will be dependent on the underlying cause. Obstructive causes may require removal of a gallstone through Endoscopic Retrograde CholangioPancreatography (ERCP) or stenting of the common bile duct.
Symptomatic treatment is often needed for the itching caused by hyperbilirubinaemia. An obstructive cause may warrant cholestyramine (acting to increase biliary drainage), whilst other causes may respond to simple anti-histamines.
Identify and manage any complications where possible. Monitor for coagulopathy, treating promptly (either vitamin K or fresh frozen plasma (FFP) is needed) if any evidence of bleeding or rapid coagulopathy, and treat hypoglycaemia orally if possible (otherwise 5% dextrose is needed).
Where patients become confused from decompensating chronic liver disease (‘hepatic encephalopathy’), laxatives (lactulose or senna) +/- neomycin or rifaximin may be used, in attempt to reduce the number of ammonia-producing bacteria in the bowel.
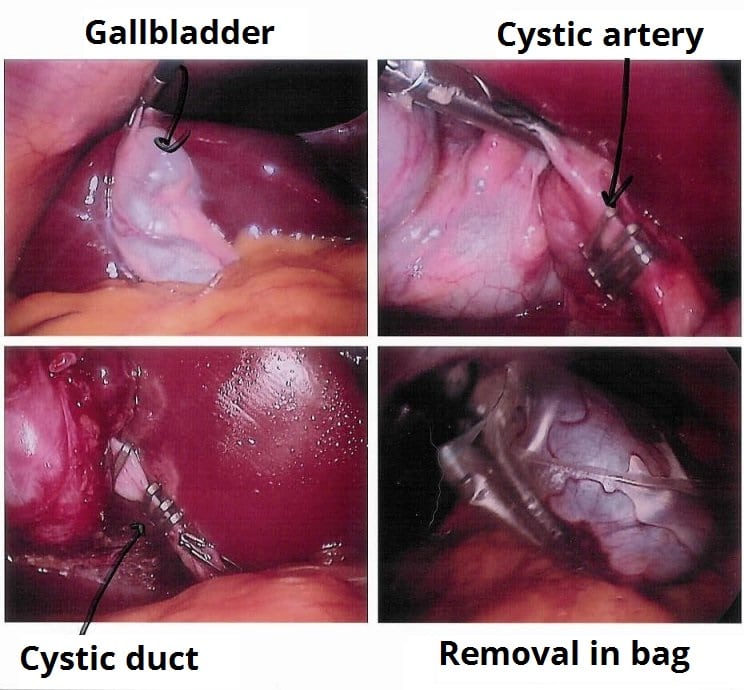
Figure 3 – Images from a laparoscopic cholecystectomy
Key Points
- Jaundice refers to the yellow discolouration of the sclera and skin that is due to hyperbilirubinaemia
- Causes can be broken down into pre-hepatic, hepatocellular, and post-hepatic
- Most cases will warrant initial blood tests and ultrasound imaging, however this should be tailored to the clinical presentation
- Definitive treatment of jaundice will be dependent on the underlying cause
- Ensure to monitor for complications, such as coagulopathy, encephalopathy, or infective sequelae