Pneumonia is defined as a lower respiratory tract infection with accompanying consolidation visible on chest x-ray. There are four main types of pneumonia:
- Community-acquired pneumonia (CAP)
- Hospital-acquired pneumonia (HAP)
- Aspiration pneumonia
- Immunocompromised pneumonia
In the post-operative setting, hospital-acquired pneumonia is the predominating type. HAP is a pneumonia that has onset >48hrs since hospital admission and was not present on admission.
Whilst incidence varies across countries, they remain a major burden on healthcare services.
Aetiology
Surgical patients are predisposed to developing lower respiratory tract infections due to a combination of:
- Reduced chest ventilation – reduced mobility in bedridden patients results in an inability to fully ventilate their lungs, leading to accumulation of fluid secretions which subsequently become infected
- Change in commensals – the hospital environment microflora will vary compared to what the patient may normally be exposed to, nor have immunity to
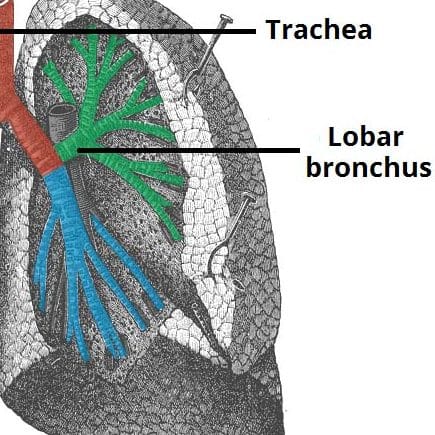
- Common pathogens (Fig. 1) for HAP include E. coli, S. aureus (including MRSA), S. pneumoniae, and Pseudomonas
- Debilitation – many patients undergoing surgery are likely to be sick or have several co-morbidities, compromising their immune systems and predisposing to pulmonary infections
- Intubation – patients undergoing major surgery may need a stay in ICU and require intubation and ventilation, a major risk factor for a HAP
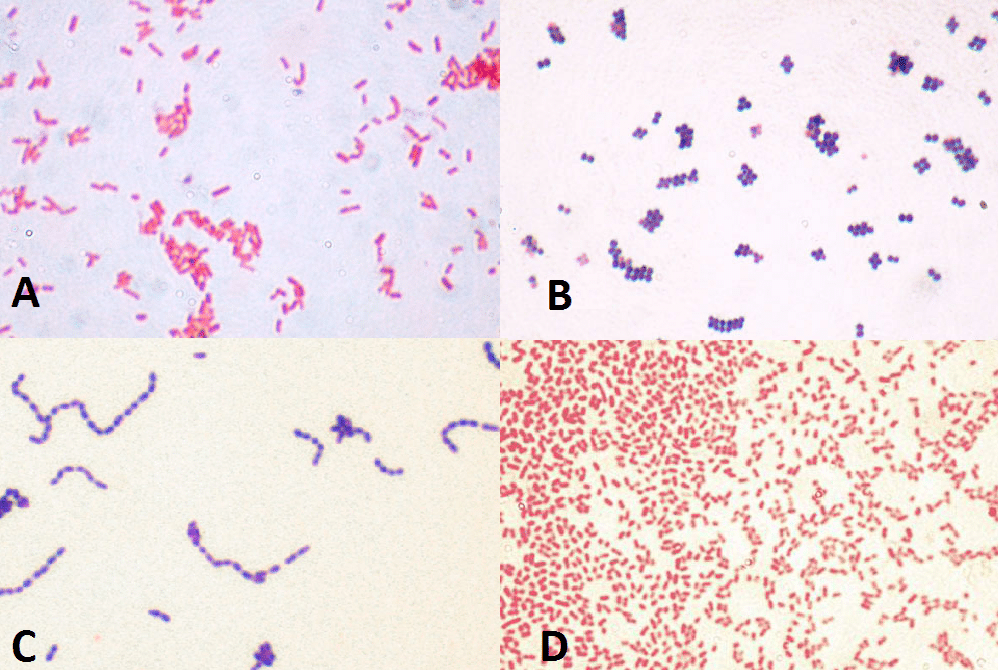
Figure 1 – Common causes of HAP under Gram Stain (A) E. coli (B) MRSA (C) S. pneumonia (D) P. aeruginosa
Ventilator Associated Pneumonia
A ventilator associated pneumonia (VAP) is a hospital acquired pneumonia that occurs >48 hours after tracheal intubation. It is the most common hospital acquired infection in patients receiving mechanical ventilation, accounting for around 50% antibiotics given in ICU setting.
They are most common in those who have an endotracheal tube in-situ, as the tube interferes with the normal protective upper airway reflexes, prevents effective coughing, and encourages aspiration of contaminated pharyngeal contents.
Risk Factors
Risk factors for developing hospital-acquired pneumonia include:
- Age
- Smoking (current or previous)
- Known respiratory disease or recent viral illness
- Poor mobility (either baseline or post-operatively)
- Mechanical ventilation
- Immunosuppression
- Underlying co-morbidities, such as diabetes mellitus or cardiac disease
Clinical Features
Patients with hospital-acquired pneumonia classically present with a combination of cough (productive or non-productive), dyspnoea, or chest pain.
However, many post-operative patients may not present as ‘clear-cut’ as this, due to factors such as intubation, reduced consciousness, or other co-morbidities. Indeed, the only clinical features may be a general malaise, pyrexia, or impaired cognition.
On examination, patients may have a reduced oxygen saturation, increased RR or HR, pyrexial, or with features of a septic response. Bronchial breath sounds (localised or diffuse) and inspiratory crackles may be heard on auscultation, associated with a dull percussion note.
Differential Diagnosis
The differential diagnoses for pneumonia include acute heart failure or acute coronary syndrome, PE, asthma or COPD exacerbation, pleural effusion or empyema, and psychological (e.g. anxiety disorder).
Investigations
Laboratory Investigations
Any suspected pneumonia should have routine bloods (FBC, CRP, and U&Es) taken, which may show evidence of an inflammatory response (raised WCC and CRP).
An arterial blood gas may be required in severe cases of oxygen desaturation; this may show a type 1 respiratory failure, or a type 2 failure (if exacerbating pre-existing COPD).
If the cough is productive, a sputum sample should be taken for culture. Any signs of a severe infection or sepsis should warrant blood cultures being taken during times of pyrexia.
Imaging
Patients with a suspected HAP will require a chest x-ray (CXR) to confirm the infection, presenting as consolidation*, either lobar or bronchopneumonia (Fig. 2).
If a sputum sample is unobtainable, severe or non-responding infections may require a bronchoalveolar lavage, yet you should gain specialist advice before requesting this.
*Consolidation can be differentiated from other shadowing on a CXR by the presence of air bronchograms
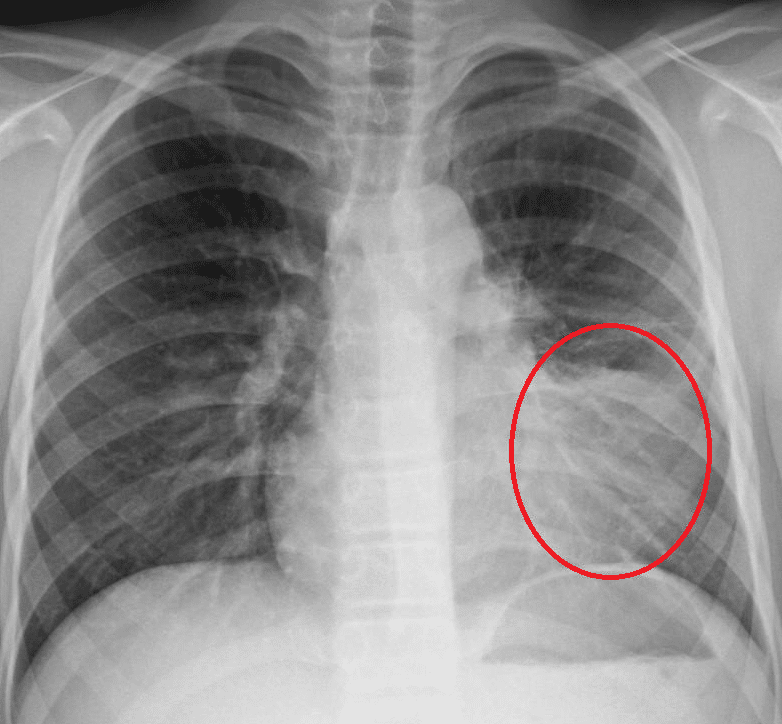
Figure 2 – A CXR showing left lower zone consolidation
CURB-65 Score
The severity of a community-acquired pneumonia can be graded based on the CURB-65 score. A score 0-1 is mild, 2 is moderate, and ≥3 is severe.
|
Clinical Criteria |
Points |
| Confusion |
1 |
| Urea >7.0mmol |
1 |
| Respiratory rate >30 |
1 |
| Systolic <90 or diastolic <60 |
1 |
| Age >65 |
1 |
Whilst the CURB-65 score can be useful in cases of CAP, its applicability to HAP is limited and other parameters and factors should guide management
Management
All patients should receive appropriate O2 therapy as indicated, targeting ≥94% saturation (or 88-92% in those at risk of hypercapnic respiratory failure). Any evidence of sepsis or septic shock should be managed and treated accordingly (discussed here).
Confirmed pneumonia should be treated with empirical antibiotics, pending sensitivities. Antibiotic choice should be guided by local policy; an example regimen is:
- Mild: Co-amoxiclav 625mg oral TDS
- Moderate: Co-amoxiclav 625mg oral TDS
- Severe: Tazocin 4.5g TDS IV
Prevention
Any post-operative patients with prolonged bedrest or reduced mobility are at risk of developing HAP (secondary to fluid stasis in the pulmonary tissue). The best practice is for post-operative patients to have chest physiotherapy to increase lung ventilation and reduce fluid stasis.
Complications
The major complications of pneumonia are:
- Pleural effusion
- Empyema
- Respiratory failure
- Sepsis
Aspiration Pneumonia
Aspiration of the gastric contents into the pulmonary tissue will result in a chemical pneumonitis. However, this is not necessarily an infection, as only if any oropharyngeal bacteria are aspirated into the lung tissue as well will a lung infection result.
Classically, any aspirated content will affect the right middle or lower lung lobes, due to the anatomy of the bronchi (Fig. 3).
In surgical patients, the main risk factors for an aspiration are:
- Reduced GCS (e.g. secondary to anaesthesia)
- Iatrogenic interventions (e.g. misplaced NG tube)
- Prolonged vomiting without NG tube insertion
- Underlying neurological disease
- Oesophageal strictures or fistula
- Post-abdominal surgery
Much of the clinical features and investigations for an aspiration pneumonia will be the same as for HAP. Importantly, aspiration pneumonia should be suspected over a pneumonitis if there is evidence of an infective process developing.
Management is mainly preventative, identifying the patients who are at an increased risk of aspirating and placing suitable precautions (e.g. NG tube feeding) in place until suitable. This will require involvement from both the nursing staff and the Speech and Language Therapists (SALT).
Any pneumonitis only needs supportive measures, however an aspiration pneumonia will need antibiotic therapy, similar to that of HAP. Suction of any aspirated contents is rarely performed as has no real benefit to overall outcomes.
Key Points
- Surgical patients are often predisposed to developing lower respiratory tract infections
- Ensure to obtain routine bloods, suitable imaging, and appropriate cultures for all suspected cases
- Following local antibiotic policy to guide management
- Complications of pneumonia are pleural effusion, empyema, respiratory failure, and sepsis