Introduction
An anastomotic leak can be defined as “a leak of luminal contents from a surgical join“. They are an important complication to recognise following gastrointestinal surgery when an anastomosis has been formed.
Early diagnosis and treatment of an anastomotic leak is essential. Anastomotic leaks can result in significant contamination of the abdomen cavity* with luminal contents, leading to the development of severe sepsis and progression to multi organ failure and even death.
Essentially, any patient who is not progressing as expected or who deteriorates after surgery should be considered to have an anastomotic leak until proven otherwise.
In this article, we shall look at the risk factors, clinical features, and management options of an anastomotic leak.
*An anastomosis following an oesophagectomy may be within the thoracic cavity, not necessarily the abdominal cavity, therefore these leaks will result in an intra-thoracic contamination
Risk Factors
There are several factors that increase the risk of an anastomotic leak:
- Patient Factors
- Medication (e.g. corticosteroids, immunosuppressants)
- Smoking or alcohol excess
- Diabetes Mellitus
- Obesity or malnutrition
- Surgical factors
- Emergency surgery
- Extended operative time
- Peritoneal contamination (e.g pus, faeces)
- Oesophageal-gastric anastomosis or colo-rectal anastomosis
Clinical Features
If a patient develops an anastomotic leak, this will usually occur between post-operative days 3 to 5, however realistically they can occur any time before or after this period.
Patients will usually present with worsening abdominal pain and clinical features of sepsis. However, certain patients may present with more subtle signs, such as a prolonged ileus – as a rule, any patient not progressing appropriately post-operatively with an anastomosis should be considered to have an anastomotic leak until proven otherwise.
On examination, patients will have a tender abdomen, either localised and generalised, with or without signs of peritonism, depending on degree on contamination. Left untreated, patients will develop worsening signs of sepsis.
Investigations
All patients with a suspected anastomotic leak should have urgent blood tests performed, including a FBC, CRP, and clotting screen. An arterial blood gas should be sent to assess pH and lactate.
Definitive investigation for a suspected anastomotic leak is with an urgent CT scan with intravenous contrast. In such cases, this will assess for the presence of gas or enteric contents outside the lumen at the site of the anastomosis, suggestive of a leak.
CT scans can be supplemented with oral contrast or contrast enema, depending on the location of the anastomosis, to aid with the diagnosis in unclear cases. When given, any contrast evident outside the bowel lumen will confirm the diagnosis.
Management
Once an anastomotic leak has been diagnosed, the key principles in management relate to timely resuscitation and control of contamination.The management varies depending on the extent of the leak, extent of contamination, and physiological status of the patient.
Ensure the patient is nil by mouth (NBM) and start broad-spectrum antibiotic cover. Prescribe resuscitative intravenous fluids and insert a urinary catheter to enable monitoring of fluid balance.
Whether the leak is managed operatively or otherwise, it is essential to ensure appropriate nutritional support is considered, as certain patients may require total parenteral nutrition for a short period.
Definitive Management
Minor anastomotic leaks may be managed conservatively. Small peri-anastomotic collections in a systemically well patient may be managed with intravenous antibiotics and bowel rest, with percutaneous drains inserted if appropriate.
Endoluminal vacuum therapy (e.g. Endo-SPONGE®) can be used in select patient with certain leaks, e.g. small leak in a low rectal anastomosis.
Patients who are systemically unwell, signs of pertonism, and/or with large leaks will require surgical intervention to ensure appropriate source control. This will typically require a laparotomy, washout of the contamination, and refashioning of the anastomosis and/or formation of a defunctioning proximal stoma.
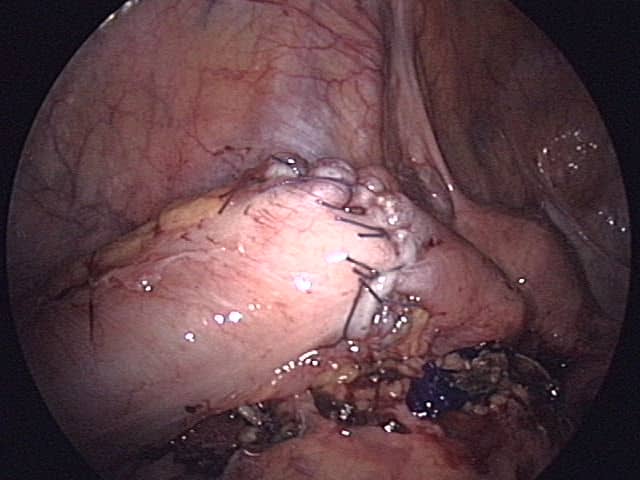
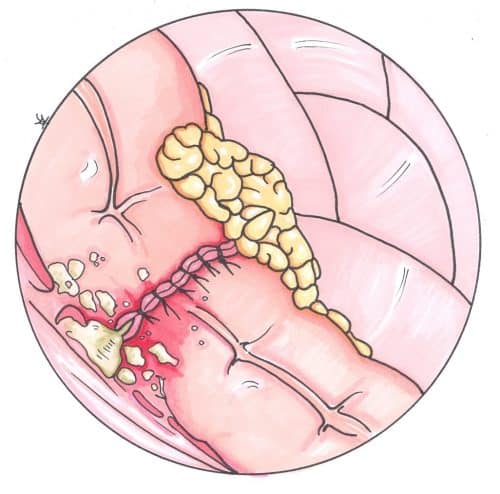
Figure 2 – A hand-sewn anastomosis of the sigmoid colon
Key Points
- Anastomotic leaks are defined as “a leak of luminal contents from a surgical join”
- They can present with abdominal pain and fever, typically 3-5 days post-operatively
- Definitive investigation is made via CT scanning with contrast
- Management is with bowel rest, intravenous antibiotics, and potential surgical intervention