Introduction
Adhesions are fibrous bands of scar tissue. Many occur secondary to previous surgery or intra-abdominal inflammation (particularly pelvic)*, however they can also be congenital.
They are one of the main causes of small bowel obstruction, accounting for around 60% of cases, and can be associated with female infertility and chronic pelvic pain.
The incidence of small bowel obstruction was highest following lower gastrointestinal surgery or paediatric surgery, and the lowest in upper gastrointestinal surgery and urological surgery.
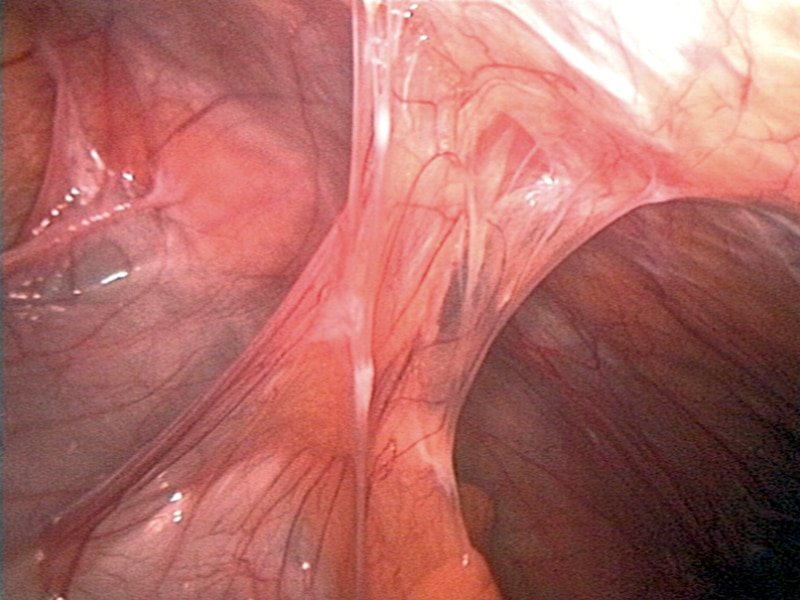
Figure 1 – Bowel adhesions, as seen on laparoscopy, causing a small bowel obstruction
Clinical Features
Adhesions themselves are generally asymptomatic. Rather, it is the effect of the adhesions that present with clinical features, such as that of obstruction, infertility, or chronic pelvic pain.
Investigations and Management
Much of the work-up required for suspected bowel adhesions is directed to that of the subsequent pathology that has developed. For those in uncomplicated bowel obstruction, conservative management should be attempted initially, the mainstay of which is tube decompression
Additionally, the patient should be kept nil-by-mouth, prescribed intravenous fluids, and provided with adequate analgesia. Gastrograffin can be trialed in uncomplicated cases, however should be avoided in cases of closed loop obstruction or suspected ischaemia.

Figure 2 – Small bowel obstruction, as seen on abdominal radiograph
Surgical Management
Surgical intervention in adhesional bowel obstruction is warranted* in any patient with clinical features of ischaemia or perforation, or failed conservative treatment. In patients that require surgical management, early intervention is preferable, as delays have been shown to lead to increased rates of post-operative complications, prolonged length of stay, and mortality.
Whilst open surgery for adhesiolysis is still performed in many cases, laparoscopic management for bowel adhesions is becoming the mainstay, due to improved post-operative outcomes. Often technically challenging due to the distension of the bowel (and therefore increased risk of iatrogenic injuries to the bowel), consequently there should be a low threshold for conversion to open approach in extensive disease.
Prevention
There are no devices currently able to totally prevent adhesion formation after abdominal surgery. Correct surgical technical and reducing intraperitoneal organ handling remain the mainstay of reducing bowel adhesion formation.
Key Points
- Bowel adhesions are a major cause of small bowel obstruction, accounting for around 60% of cases
- For those warranting surgical management, adhesiolysis can be performed laparoscopically or via an open approach
