Constipation is a common post-operative complaint and is one that all doctors across all specialities should assess for regularly.
It is defined as a condition in which a patient has infrequent bowel movements (<3 a week), often with hard, dry stools that may be painful and difficult to pass.
In this article, we shall look at the aetiology*, clinical features, and management of post-operative constipation.
*It is worth noting that following abdominal surgery, there are more significant causes to consider in those not passing flatus or stool, and should be approached differently than outlined in this article
Aetiology
The main causes of constipation that are seen on the surgical ward include:
- Physiological – due to factors such as a low fibre diet, poor fluid intake, or low physical activity
- Iatrogenic – medications such as opioid analgesia, anticonvulsants, iron supplements, or antihistamines
- Pathological – such as hypercalcaemia, hypothyroidism, or neuromuscular disease
- Functional – from painful defecation (such as anal fissures)
Following abdominal procedures, post-operative ileus can also be a common cause in the post-operative setting. Any patient with absolute constipation and associated features of bowel obstruction should be considered as such until proven otherwise
Clinical Features
Constipation can present with lower abdominal pain. In severe cases, patients may also present with abdominal distension, nausea and vomiting, or decreased appetite.
Most patients will have no clinical signs on examination; only severe cases are likely to have abdominal distension or tenderness (both secondary to faecal impaction).
A Digital Rectal Examination (DRE) is essential for any patient with constipation to assess the degree of faecal impaction.
Investigations
Most cases of post-operative constipation are benign in nature and can be made as a clinical diagnosis, with no further investigations required. However any features should suggestive of an underlying sinister pathology will require endoscopy.
If no cause can obviously be identified or it is severe/resistant to treatment, routine bloods (such as TFTs or serum Ca2+) may be requested.
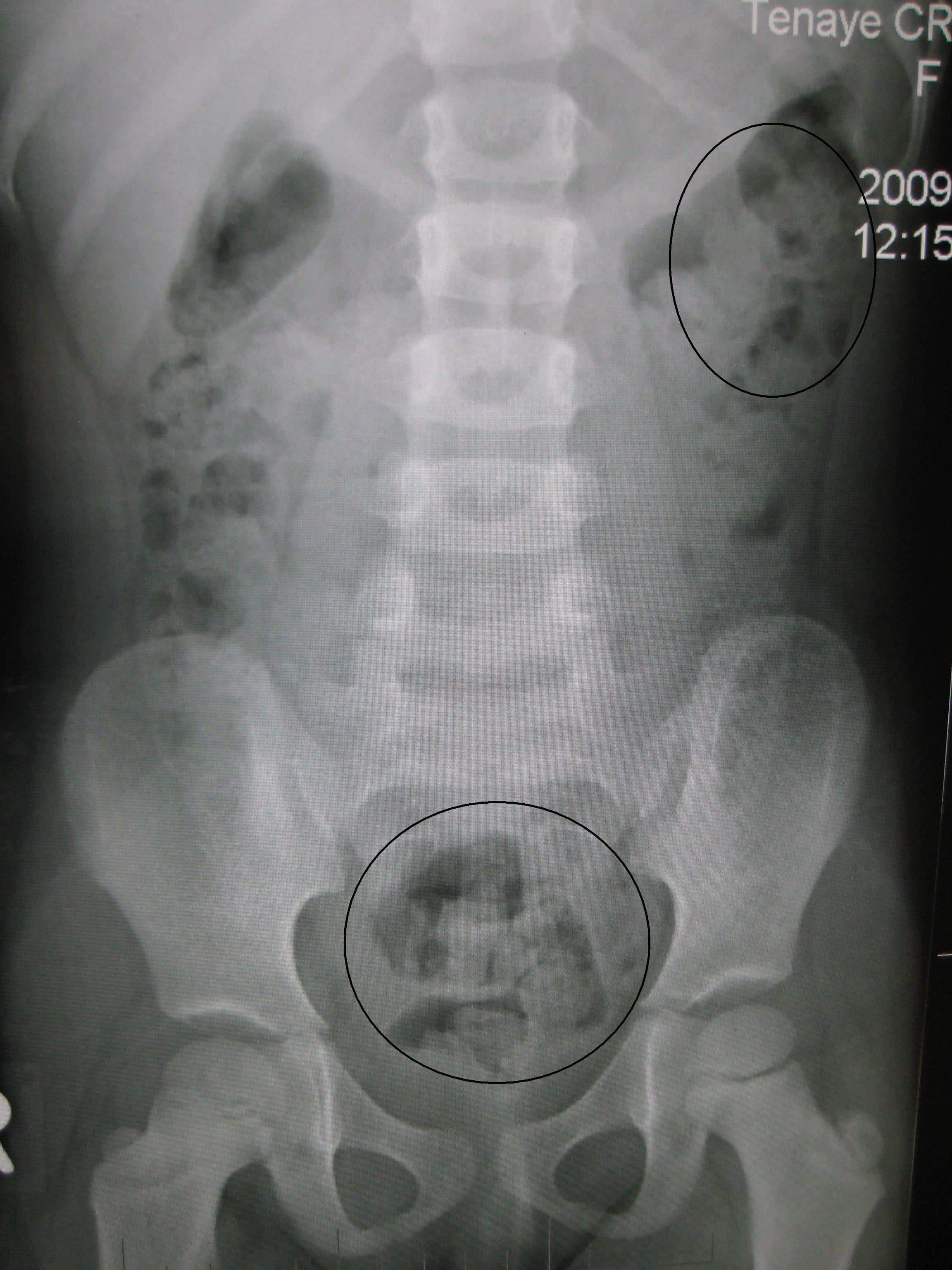
Abdominal plain film radiographs or CT scans are generally not indicated in routine cases; imaging may indeed show faecal impaction (Fig. 2), yet this is not an indication for the image request.
Management
In the vast majority of cases, post-operative constipation can be treated via conservative measures alone. These include ensuring adequate hydration and sufficient dietary fibre, treating the underlying cause, and encouraging early mobilisation.
Pharmacological
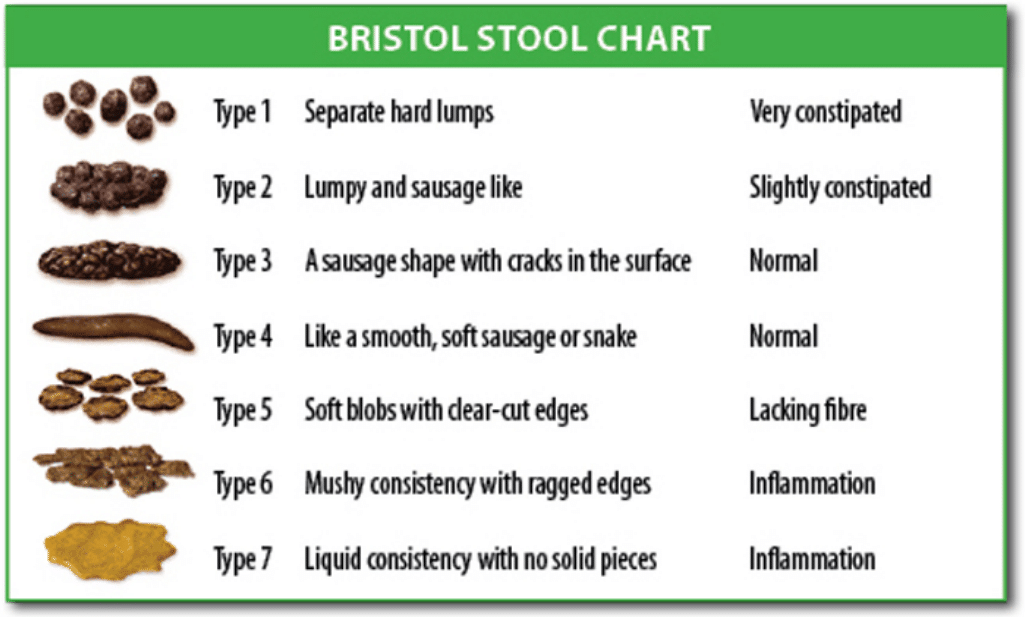
Laxatives can be used if the patient remains constipated; the choice of laxative depends upon the suspected underlying cause and stool consistency on PR examination*.
The major types of laxatives are:
- Osmotic laxatives – increase the amount of fluid in the bowel thereby softening stool. e.g. lactulose, movicol
- Stimulant laxatives – stimulate the bowel to contract thus expelling faeces. e.g. senna, picosulphate
- Bulk forming laxatives – help stool to retain water thereby softening stool. e.g. ispaghula husk
- Rectal medications – glycerin suppository (stimulant), phosphate enema (stimulant)
Patients with a hard stool and chronic constipation issues will benefit from a stool-softening laxative, such as movicol or lactulose, but may require glycerine suppositories to help soften the rectal stool initially.
Patients with post-operative ileus, opioid-induced constipation, or a soft stool will benefit from a stimulant laxative, such as senna or picosulphate.
*In resistant cases, additional therapy can be given via manual evacuation.
Prophylaxis
Opioid analgesia should be avoided where possible and other opioid-sparing agents used. Prophylactic stimulant laxatives, such as senna, should be used for patients on opioid analgesia, especially in the elderly.
Key Points
- Constipation is a common post-operative complaint
- Most cases are multi-factorial and all should be addressed to ensure optimal management
- Ensure to perform a digital rectal examination on all cases of constipation
- Most cases can be treated conservatively, with use of laxatives as required, tailored to the underlying cause of the constipation