Introduction
Post-operative ileus describes a deceleration or arrest in intestinal motility following surgery. It is classified as a functional bowel obstruction and is very common, particularly after abdominal surgery or pelvic orthopaedic surgery.
Remember however that although innocent in the majority of patients, it can be a sign of other intra-abdominal pathology*, in particular a collection or anastomotic leak (as pus or faeces will irritate the bowel and often cause it to cease functioning).
Post-operative ileus has been shown to lengthen hospital stay and increase hospital costs; indeed, the overall annual expenditure in the US secondary to postoperative ileus is around $750 million to $1 billion.
Risk Factors
- Patient Factors
- Increased age
- Electrolyte derangement (e.g. Na+, K+and Ca2+ derangement)
- Neurological disorders (e.g. Dementia or Parkinson’s Disease)
- Use of anti-cholinergic medication
- Surgical Factors
- Use of opioid medication
- Extensive intra-operative intestinal handling
- Peritoneal contamination (by free pus or faeces)
- Intestinal resection
Clinical Features
A post-operative ileus is simply a delay in the return of normal bowel function. As a result, the symptoms of post-operative ileus may be the same as those of a mechanical obstruction.
Common presenting features therefore are:
- Failure to pass flatus or faeces
- Sensation of bloating and distention
- Nausea and vomiting (or high NG output)
On examination, there will be abdominal distention and absent bowel sounds (whereas in mechanical obstruction there are classically “tinkling” bowel sounds present)
Investigations
In the patients with suspected post-operative ileus, the aim of the investigations are to rule out more serious pathologies and determine any underlying cause.
Initial routine bloods should be taken, including FBC and CRP (to check inflammatory markers), and U&Es (as fluid shifts can occur within the adynamic bowel leading to AKI). The patient’s electrolytes, including Ca2+, PO₄³⁻, and Mg2+, should also be checked and corrected accordingly.
A CT scan abdomen and pelvis (often with oral contrast) will confirm the diagnosis (Fig. 1) and importantly also rule out any intra-abdominal collections or anastomotic leaks.
Management
As long as serious pathology (e.g. anastomotic leak) has been excluded, the management of post-operative ileus is often conservative.
Any established postoperative ileus should be initially managed with:
- Nil-by-mouth (NBM), ensuring adequate intravenous fluids prescribed
- Start a strict fluid-balance chart to monitor input-output
- Insertion of a nasogastric tube (Fig. 2), on free drainage with regular aspirations
- Daily bloods, including electrolytes
- Correct any electrolyte abnormalities and monitor for acute kidney injury
- Encourage mobilisation as tolerated
- Reduce opiate analgesia and any other bowel mobility reducing medication
It is important to warn patients that once it does settle, they may well have very watery stool for the first few bowel movements.
In patients with a prolonged ileus, consider early total parenteral nutrition (TPN) to ensure optimal nutrition is maintained
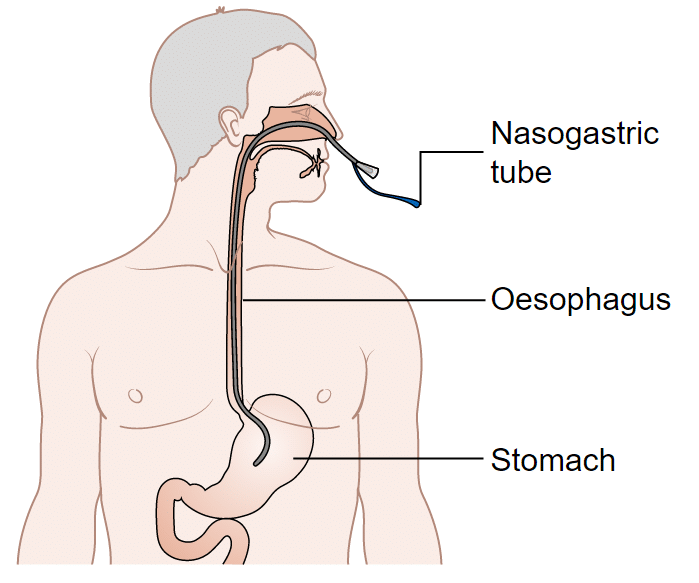
Figure 2 – A nasogastric tube should be inserted as part of the management for post-operative ileus
Prophylactic Measures
To reduce the risk of developing post-operative ileus, preventive steps include:
- Minimise intra-operative intestinal handling
- Avoid fluid overload (causing intestinal oedema)
- Minimise opiate use
- Encourage early mobilisation
Key Points
- Post-operative ileus describes a deceleration or arrest in intestinal motility following surgery
- Both patient and surgical factors increase the risk of it developing
- Mainstay of management is nil by mouth, nasogastric tube insertion, and intravenous fluids
- Ensure early patient mobilisation, ensure to correct any electrolyte abnormalities, and avoid any medication that can reduce bowel motility
- CT imaging may be warranted, especially in prolonged cases, to exclude more serious intra-abdominal pathologies as an underlying cause

