Introduction
An incisional hernia is the protrusion of the contents of a cavity (usually the abdomen) through a previously made incision in the compartment’s wall.
They occur (by definition) after an operation, and unfortunately are a common complication of abdominal surgery, with prevalence following laparotomy around 5.2% at 1year (nearly 25% by 2yrs).
In this article, we shall look at the risk factors, clinical features and management of an incisional hernia.
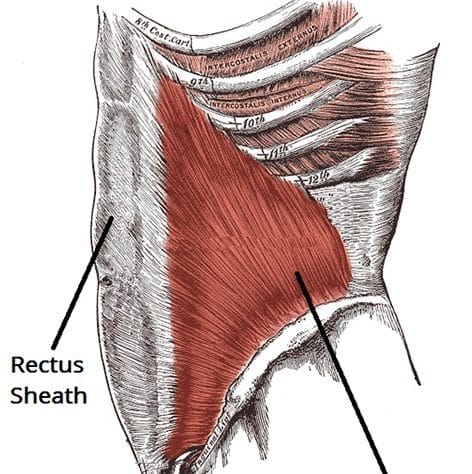
Pathophysiology
The layers of the anterior abdominal wall are normally strong and act to maintain the integrity of the abdominal cavity. However, once these layers are interrupted by a surgical incision, their continuity is disrupted and become structurally weakened.
In the presence of increased intra-abdominal pressure and potential risk factors (such as smoking or obesity), the contents of the abdomen are able to herniate through the weakness, forming an incisional hernia.
As with any hernia, complications can occur, such as incarceration, strangulation, or obstruction.
Risk Factors
The risk factors for incisional hernia following abdominal surgery include (ranked by relative risk):
- Emergency Surgery
- Emergency surgery carries double the risk of elective surgery
- BMI >25
- Obese patients are more likely to develop an incisional hernia
- Midline incision
- There is a 74% risk increase compared to non-midline
- Post-operative wound infection
- This increases incisional hernia risk by 70%
- Diabetes Mellitus, Connective Tissue Disorders, or Steroid Use
- Advancing age
- Current Smoker
Clinical Features
The characteristic clinical feature of an incisional hernia is a reducible, soft and non-tender swelling at or near the site of a previous surgical wound. If the hernia is incarcerated, it can become painful, tender, and erythematous.
On examination, a mass is palpable at or near the site of the surgical incision, which may be reducible into the abdominal cavity (depending on its severity). Ensure to also check the groins for the other hernial orifices.
Ensure to check for clinical features of obstruction and ischaemia.
Investigations
In most cases of incisional hernia, the diagnosis is made on a clinical basis. However, often radiological imaging can be used to confirm the diagnosis, most commonly CT imaging* (Fig. 2).
*CT imaging can not only confirm the diagnosis, but in large incisional hernia can help plan operative management
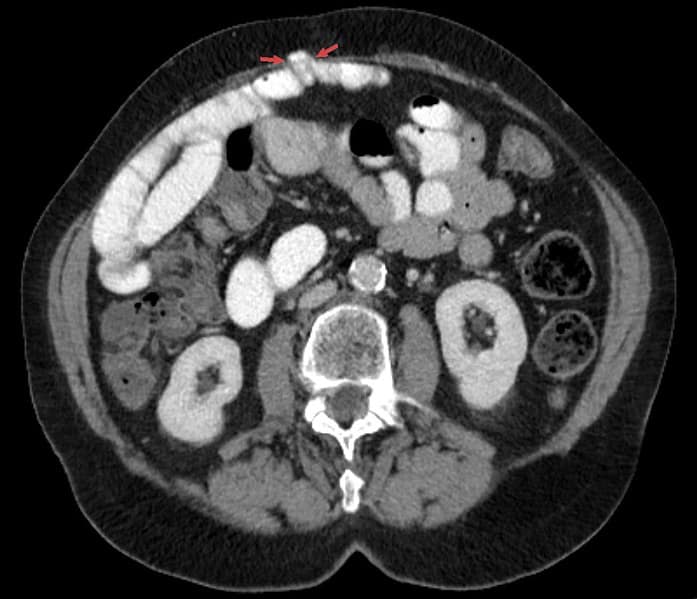
Figure 2 – CT imaging showing a small bowel loop within an abdominal incisional hernia at the midline (arrow)
Management
The management of an incisional hernia should be considered on a case-by-case basis. The majority of incisional hernias are asymptomatic and can be managed electively.
Surgery is typically indicated in patients with symptomatic hernias who are clinically fit enough for surgery. The size of the hernia and the abdominal wall defect, the clinical features, the patient’s age and co-morbidities, and the patient’s preferences should all be taken into account.
Incisional hernias can be repaired using a variety of techniques, including suture repair (for very small hernias), laparoscopic mesh repair, and open mesh repair. For large incisional hernia, varying degrees of abdominal wall reconstruction may be required.
Prognosis
Many incisional hernias remain asymptomatic life-long; 6-15% of them will incarcerate and 2% will progress to strangulation.
Key Points
- An incisional hernia is a hernia that occurs through a previously made incision in the abdominal wall
- Diagnosis is typically clinical, however imaging can help to confirm the diagnosis and elucidate the anatomy
- Management is decided on a case-by-case basis, however if suitable most patients will warrant surgical intervention