Introduction
Wound dehiscence is where a wound fails to heal, whereby the wound re-opens in the days following surgery. This is most common following abdominal surgery.
It can be divided into two clinical entities (Fig. 1):
- Superficial dehiscence – the skin wound alone fails, with the rectus sheath remaining intact
- Often occurs secondary to local infection, poorly controlled diabetes mellitus, or poor nutritional status
- Full thickness dehiscence – the rectus sheath fails to heal and “bursts”, with protrusion of abdominal content (often termed a “burst abdomen”)
- This may occur secondarily to raised intra-abdominal pressure (e.g. patients with ileus), poor surgical technique, or if the patients is critically unwell
Wound dehiscence is a costly post-operative complication and thus identification and appropriate management of the condition is key.
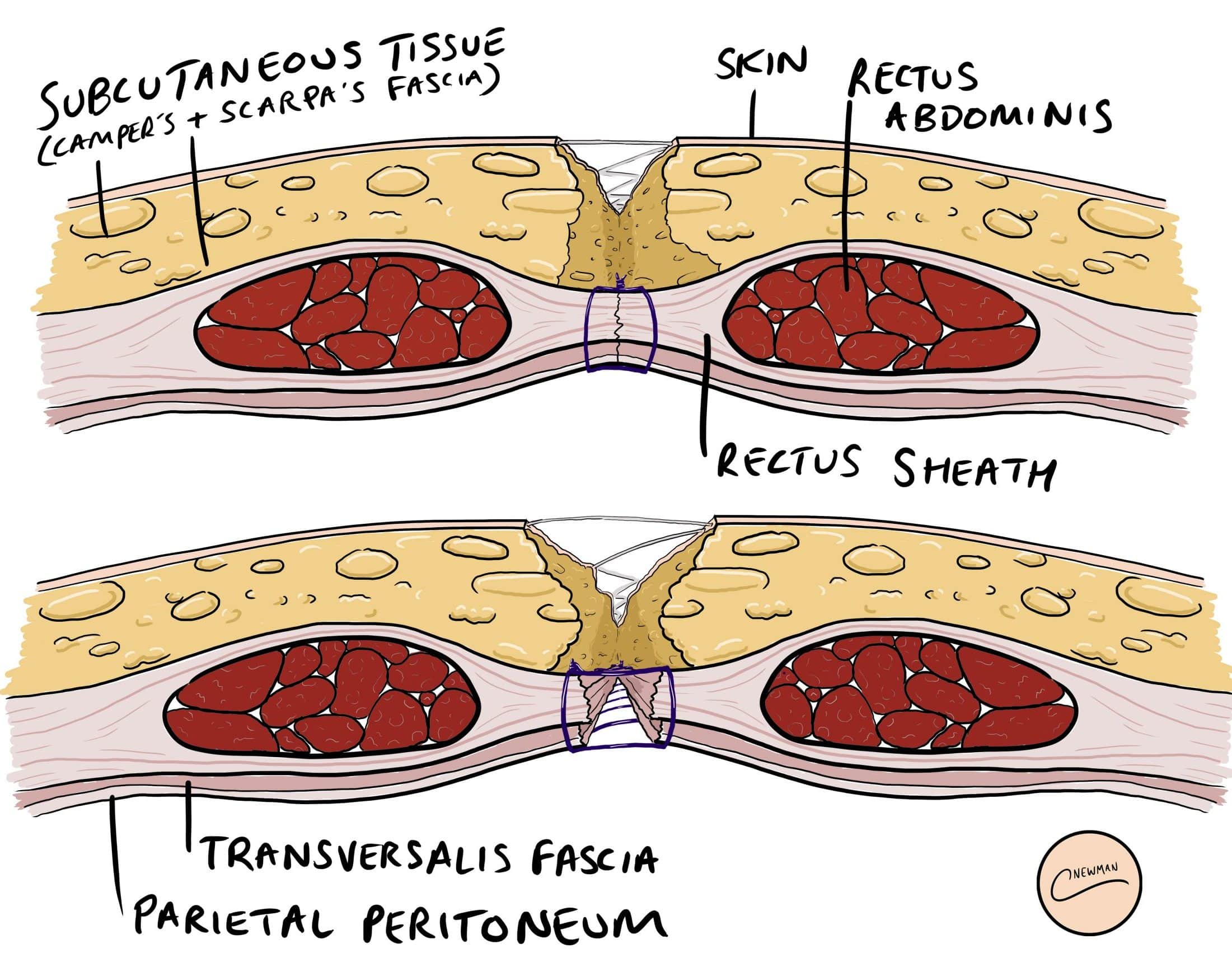
Figure 1 – Schematic demonstrating layers involved in (A) Superficial Dehiscence (B) Full Thickness Dehiscence
Aetiology
The most common cause of wound dehiscence is surgical site infection.
However, risk factors can be divided into patient, intra-operative, and post-operative factors (Table 1)
| Patient Factors | Intra-Operative Factors | Post-Operative Factors |
|
|
|
Table 1 – Risk Factors for Wound Dehiscence
Clinical Features
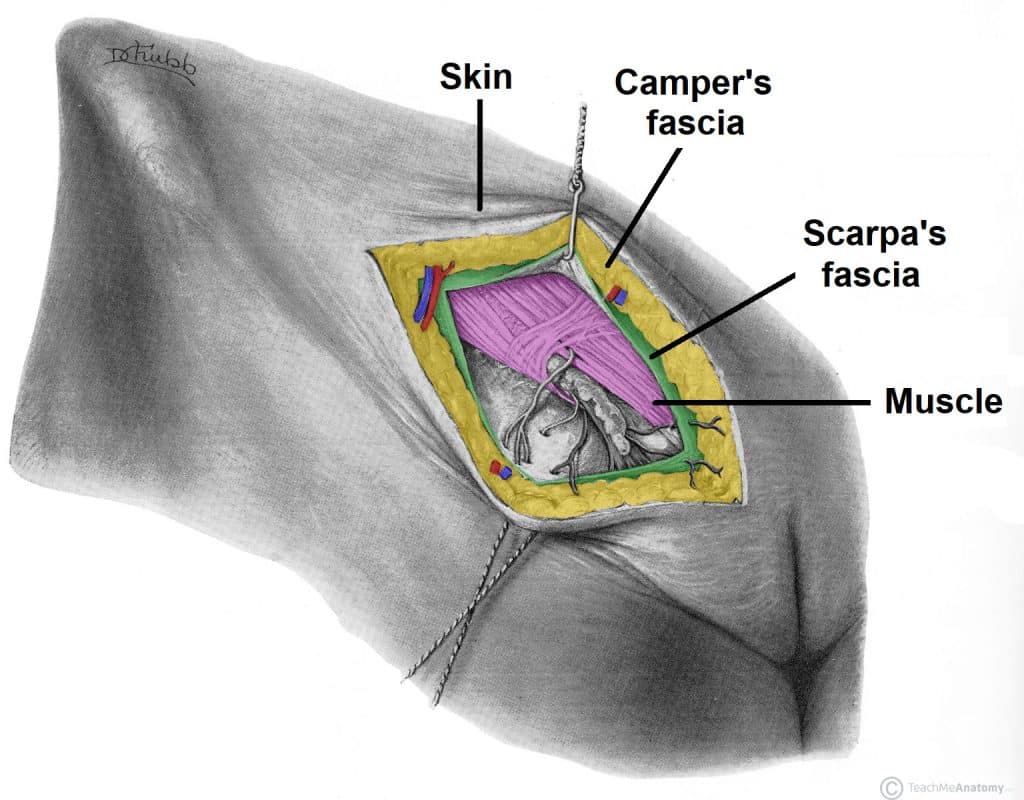
For a superficial wound dehiscence, the most evident feature is the visible opening of the wound (Fig. 2), healing poorly following the operation; this typically happens around 5-7 days post-operatively. This may be associated with surrounding erythema or purulent discharge, secondary to a concurrent surgical site infection (SSI).
For a full thickness dehiscence, the skin can often be intact however there is a new bulging of the wound and an increased seepage of pink serous or blood-stained fluid appearing from the wound. A sudden increase in wound discharge should be considered as deep dehiscence until proven otherwise*.
In severe cases of full thickness dehiscence (“burst abdomen”), there is a visible protrusion of abdominal contents (typically omentum or bowel) through the wound.
*Such a presentation will mandate removal of the skin clips / sutures at the area of maximal leakage and physically examining the rectus sheath with your finger or a wound swab to check it is still intact
Investigations
The diagnosis of wound dehiscence is clinical. For cases with concurrent surgical site infection, wound swabs should be taken for culture at the wound site.
Management
A superficial wound dehiscence can typically be treated with conservative measures only. Any underlying cause (e.g. SSI) should be managed accordingly. Simple wound care is all that is required in the majority of cases, with regular wound packing and cleaning with sterile saline.
The patient should be advised the wound will heal by secondary intention as a result of the dehiscence and that this can take several weeks. More extensive wound dehiscence may require negative pressure wound therapy to aid in healing.
Management of Full Dehiscence
For patients with a full dehiscence of a wound (“burst abdomen”), an initial A to E assessment is required, as patients with this can become very unwell. Ensure suitable analgesia is provided and start broad spectrum intravenous antibiotics as a priority. Cover the wound, along with any protruding viscera, with saline-soaked gauze as a temporising measure.
The patient will require an urgent return to theatre for re-closure of the wound. For the majority of patients, closure of the deep fascial layers (e.g. the rectus sheath) is performed using large interrupted sutures, avoiding excessive tension, followed by an extensive washout of the wound. If viscera has protruded through the wound, ensure to carefully inspect them for any signs of any injury.
In a small number of cases, primary closure of the is inappropriate or unsafe (e.g. gross abdominal sepsis, necrotising fasciitis of abdominal wall) and requires to be managed as an open abdomen (e.g. using a negative pressure dressing) or using a bridging mesh.
Prevention
Optimisation of co-morbidities pre-operatively and promptly treating any surgical site infections post-operatively remain key in the prevention of wound dehiscence. Avoiding strenuous activity in the early post-operative period (in high risks cases) and ensuring adequate post-operative nutrition are also key.
Key Points
- Wound dehiscence is the failure of a wound to close properly, divided into either a superficial wound dehiscence or full thickness dehiscence (also known as a “burst abdomen”)
- Most cases of superficial wound dehiscence are due to infection, however several other risk factors can also increase the risk
- Superficial wound dehiscence often require treatment of the underlying cause and allowing the wound to heal by secondary intention
- Full-thickness dehiscence warrants an urgent return to theatre