Introduction
Acute limb ischaemia is defined as the sudden decrease in limb perfusion that threatens the viability of the limb.
Complete or even partial occlusion of the arterial supply to a limb can lead to rapid ischaemia and poor functional outcomes within hours. Acute limb ischaemia has an incidence of around 1.5 per 10,000 person-years.
In this article, we shall look at the causes, clinical features and management of a patient with acute limb ischaemia
Aetiology
The causes of acute limb ischaemia can be classified into three main groups:
- Embolisation whereby a thrombus from a proximal source travels distally to occlude the artery (most common)
- The original thrombus source may be as a result of atrial fibrillation, post-MI mural-thrombus, abdominal aortic aneurysm, or prosthetic heart valves
- Thrombosis in situ whereby an atheroma plaque in the artery ruptures and a thrombus forms on the plaque’s cap (presenting as acute or acute-on-chronic)
- Trauma (less common), including compartment syndrome
Clinical Features
Classically, the signs and symptoms of acute limb ischaemia can be described using the 6 Ps (the first three here being the most common initial features):
- Pain
- Pallor
- Pulselessness
- Paresthesia
- Perishingly cold
- Paralysis
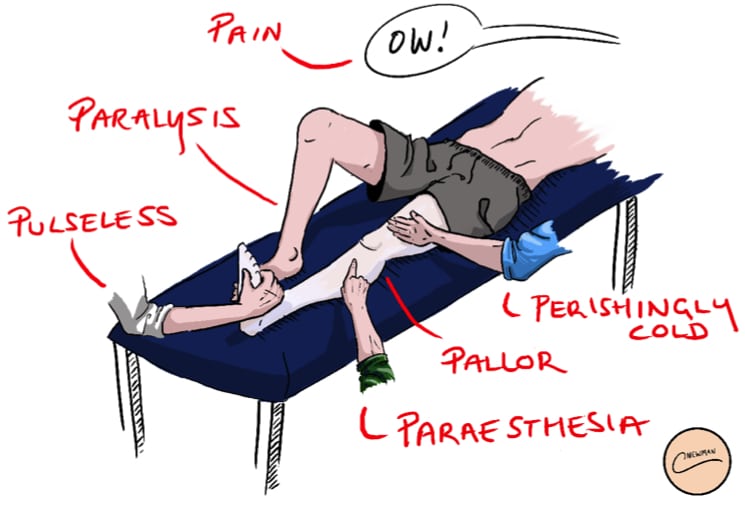
Figure 1 – The 6 Ps of Acute Limb Ischaemia
Acute limb ischaemia is often characterised by a sudden onset of these symptoms. A normal pulsatile contralateral limb is a sensitive sign of an embolic occlusion.
In the history, the causes of potential embolisation should be explored. These include chronic limb ischaemia, atrial fibrillation, recent MI (resulting in a mural thrombus), abdominal aortic aneurysm, and peripheral aneurysm.
The later the patient presents to a hospital, the more likely that irreversible damage to the neuromuscular structures will have occurred (more common >6hrs post-symptom onset), which will ultimately result in a paralysed limb (Table 1).
| Category | Prognosis | Sensory Loss | Motor Deficit | Arterial Doppler |
Venous Doppler |
| I – Viable | No Immediate threat | None | None | Audible | Audible |
| IIA – Marginally Threatened | Salvageable, if promptly treated | Minimal (toes) or none | None | Inaudible | Audible |
| IIB – Immediately Threatened | Salvageable if immediately revascularised | More than toes, rest pain | Mild/Moderate | Inaudible | Audible |
| III – Irreversible | Major tissue loss, permanent nerve damage inevitable | Profound | Profound, paralysis | Inaudible | Inaudible |
Table 1 – Clinical Categories of Acute Limb Ischemia, adapted from Rutherford et al., 2009
Differential Diagnosis
The differential diagnoses for acute limb ischaemia include critical limb threatening ischaemia, acute DVT (can present as phlegmasia cerulea dolens and phlegmasia alba dolens), or spinal cord or peripheral nerve compression.
Investigation
Routine bloods, including a serum lactate (to assess the level of ischaemia), a thrombophilia screen (if <50yrs without known risk factors), and a group and save, should be taken, along with an electrocardiogram (ECG).
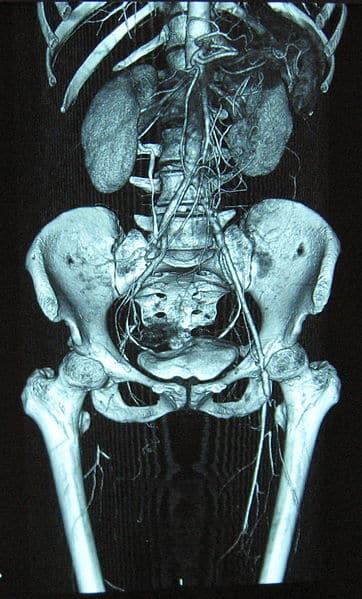
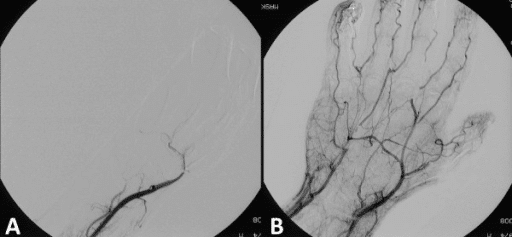
Suspected cases should be initially investigated with beside Doppler ultrasound scan (both limbs), followed by potential CT angiography (Fig. 2). If the limb is considered to be salvageable, a CT arteriogram can provide more information regarding the anatomical location of the occlusion and can help decide the operative approach (such as femoral versus popliteal incision).
Management
Initial Management
Acute limb ischaemia is a surgical emergency. Complete arterial occlusion will lead to irreversible tissue damage within 6 hours. Early senior surgical support is vital.
Start the patient on high-flow oxygen and ensure adequate intravenous access. A therapeutic dose heparin or intravenous heparin infusion should be initiated as soon as is practical.
Conservative Management
Conservative management can often be considered for those with Rutherford 1 and 2a; a prolonged course of heparin may be the most effective non-operative management of acute limb ischaemia.
Any patient started on conservative management via heparin will need regular assessment to determine its effectiveness through monitoring APPT ratio blood tests and clinical review. Surgical intervention may be warranted if no significant improvement is seen.
Surgical Intervention
Surgical intervention is mandatory for cases presenting in Rutherford 2b
If the cause is embolic, the options are:
- Embolectomy via a Fogarty catheter; this can be done over a wire using radiological guidance
- Local intra-arterial thrombolysis*
- Bypass surgery (if there is insufficient flow back), or to exclude an occluded popliteal aneurysm
If the cause is due to thrombotic disease, the options are:
- Local intra-arterial thrombolysis
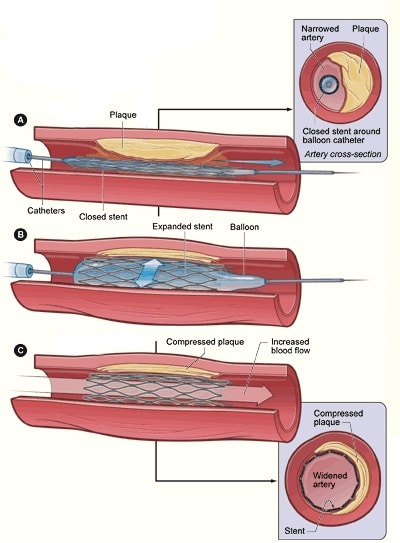
- Angioplasty (Fig. 3), likely combined with thrombolysis
- Bypass surgery
*Intra-arterial thrombolysis is often difficult to conduct within 6 hours, therefore often used for Rutherford 2a
Irreversible limb ischaemia (mottled non-blanching appearance with hard woody muscles) requires urgent amputation or taking a palliative approach.
Most post-operative cases require a high level of care, typically at a high dependency unit, due to the ischaemia reperfusion syndrome.
Long Term Management
Reduction of the cardiovascular mortality risk in this patient group is key. Promoting regular exercise, smoking cessation, and weight loss as necessary.
Most cases should be started on an anti-platelet agent, such as low-dose aspirin or clopidogrel, or even anticoagulation with warfarin or a DOAC. Any underlying predisposing conditions to the acute limb ischaemia should be treated, e.g. uncontrolled atrial firbillation.
Cases resulting in amputation will require occupational therapy and physiotherapy, with a long term rehabilitation plan discussed and transfer to an intermediate rehabilitation centre.
Complications
Acute limb ischaemia has a mortality rate of around 20%, with the 30-day mortality rate following the surgical treatment of acute limb ischaemia at 15%.
An important complication of acute limb ischaemia is reperfusion injury, whereby the sudden increase in capillary permeability can result in:
- Compartment syndrome – common following revascularisation for acute limb ischaemia, therefore fasciotomies are often done at the time of surgery to lower this risk
- Patients will typically present with calf swelling and severe pain on passive movement of the muscles; without prompt fasciotomy this will lead to muscle necrosis
- Release of substances from the damaged muscle cells, such as K+ ions causing hyperkalaemia, H+ ions causing acidosis, Myoglobin resulting in significant AKI
It is imperative that patients at risk of compartment syndrome are closely monitored and rapidly treated. Electrolyte imbalance due to reperfusion injury requires close monitoring and potentially haemofiltration.
Key Points
- Most cases of acute limb ischaemia will present with sudden onset pain and pallor, caused by either acute thrombus-in-situ or embolisation
- CT angiography is the gold-standard investigation
- A variety of treatment options are available, depending on underlying cause, regional anatomy, and co-morbid status
- Ensure to monitor for reperfusion syndrome in cases of acute limb ischaemia