Around 20% of all central nervous system tumours are spinal in origin. Spinal tumours can be very debilitating, posing a significant risk to patient morbidity and mortality. Importantly, the most common tumour type of the spine is secondary metastasis.
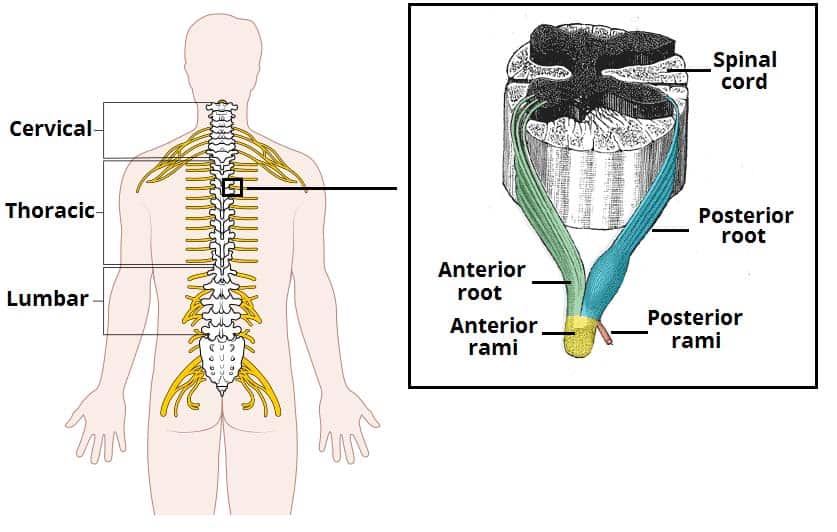
Spinal tumours can be classified into intramedullary, extramedullary, and extradural. These can be classified further into either benign or malignant. They will present with varying clinical features, with pain the most common symptom (secondary to direct compression, vascular occlusion, or invasive infiltration of the cord).
In this article, we shall look the classification, clinical features, and management of spinal cord tumours.
Classification
Spinal tumours can be intramedullary, extramedullary, and extradural. There are several subtypes, as detailed in the Appendix.
Extradural
Extradural tumours are the most common spinal tumours, arising within the vertebrae themselves. Whilst the majority are metastatic deposits, there are a small proportion that are primary, both either benign* or malignant. Enneking staging scores are used for both benign and malignant tumours respectively.
*Some benign spinal tumours are associated to spinal deformities, such as osteoid osteoma and osteoblastoma that are often associated with scoliosis
Intramedullary
Intramedullary tumours arise from within the spinal cord itself, around 60%-70% are of glial origin. These tumours are usually slow-growing in nature, with non-specific presenting symptoms. Due to the compact nature of the spinal cord, any surgical intervention on intramedullary tumours has high risk of iatrogenic injury.
Extramedullary
Extramedullary tumours arise from a range of tissues, such as nerves, blood vessels, meningeal layers, located within the space between the dura and spinal cord. They commonly present with pain, however fortunately are almost always benign and well demarcated, making them suitable for successful surgical resection.
Metastatic Spinal Tumours
The majority of spinal tumours are secondary deposits from distant primaries. The most common primaries that metastasise to the spinal cord are lung, breast, prostate, kidney and thyroid.
The main complication from metastatic spinal cord tumours is Metastatic Spinal Cord Compression (MSCC), affecting around 5-10% of all cancer patients, which can lead to permanent paralysis if untreated.
Prognosis from metastatic spinal disease can be guided by the revised Tokuhashi score, including performance status, number of extraspinal bone metastases, metastases in the vertebral body, and metastases to the major internal organs, the primary site of cancer, and evidence of spinal cord palsy to calculate an overall mean survival.
Clinical Features
The most common presenting feature is pain, typically long-standing and localised, dull in nature and potentially aggravated by supine positioning.
Those with nerve root or spinal cord compression may also develop motor symptoms (weakness or paralysis, loss of sphincter function) and sensory symptoms (paraesthesia). In malignant lesions, systemic symptoms, including weight loss or fatigue, may be present.
Ensure to complete a full peripheral neurological examination, noting levels of any neurological deficits present. Documentation of any red flags of back pain is essential.
Red Flags of Back Pain
| Age <16 years or >55 years first episode |
| History of cancer |
| Night pain |
| Progressive neurology |
| Persistent or unrelenting symptoms |
| History of trauma (especially if known osteoporotic) |
| Known immunocompromised |
Risk Factors
Certain genetic conditions increase the risk of developing spinal tumours, including Neurofibromatosis type 1 and type 2 (schwannomas), Tuberous Sclerosis (astrocytomas), Von Hippel-Lindau disease (hemangioblastomas), and Li-Fraumeni syndrome (gliomas)
Other risk factors include elevated radiation exposure, previous malignancies, and family history.
Investigations
All patients should have routine blood tests, including FBC, LFTs, CRP and ESR, and bone profile. Imaging will depend on the clinical features.
Depending on the centre, patients may initially have plain film radiographs of the affected region, however these are often poorly sensitive and specific. Bone scans, such as PET-CT imaging, can be used to evaluate for secondary metastasis to the spine.
Spinal MRI scan should be used as gold-standard imaging in suspected spinal tumour cases, providing good definition of the extent and nature of the lesion.
In cases of primary tumour, a biopsy may be required (either needle or open) to determine the tumour type and confirm the diagnosis, if not confirmed by imaging alone.
Management
The management of spinal tumours should be determined by the multidisciplinary team (MDT), with input from neurosurgeons, oncologists, and radiologists, amongst others. Management plans should be determined by the biology, location, and spread of the lesion.
In brief, many benign lesions can be simply monitored over time, with surgical intervention only if necessary, whilst malignant lesions will warrant a potential combination of surgery, adjuvant chemotherapy, and adjuvant radiotherapy (both acting to reduce tumour volume and related oedema).
Ensure patients have optimal pain management, especially with neuropathic analgesics. Patients often benefit from oral steroids, reducing tumour size and compressive symptoms.
Surgical Management
The mainstay of surgical management for suitable cases is decompression and excision. Pre-operative embolization can also be used in some settings, to aid surgical management.
There are several surgical techniques that are used, including curettage, intralesional resection (often used for benign lesions or for partial removal of inoperable malignant tumours), or en-bloc resection* (removal of the whole tumour with a layer of normal tissue)
*Main methods are vertebrectomy, sagittal resection, and resection of the posterior arch.
Key Points
- There are several types of spinal tumours that are classified by the nature and location of the lesion
- The most common presenting complaint is back pain
- Benign tumours are often monitored and resected using surgical techniques if necessary
- Malignant tumours should be treated with surgical techniques alongside adjunct therapies
Appendix
Extradural
Primary Benign Tumours
|
Tumour Subtype |
Demographic Most Affected |
Pathogenesis |
| Osteochondroma | Under 20yrs, more common in males | Overgrowth of chondrocytes and osteocytes at the growth plates |
| Hemangioma | 30-50yrs (mostly affects the thoracic and lumbar levels) | Vascular tumour composed of thick-walled vessels in a lattice-like formation |
| Langerhans cell histiocytosis | Under 20yrs, more common in males | Pathogenesis unknown; characterised by the presence of cells similar to bone marrow-derived Langerhans cells |
| Osteoid osteoma
|
Under 20yrs, more common in males (classically presents with nocturnal pain, relieved by NSAIDs) | Small lesions, composed of a nidus (dilated vessels, osteoblasts, osteoid and fibrous bone), a fibrovascular rim, and surrounding reactive sclerosis
|
| Osteoblastoma | 20-30yrs, more common in males (mostly affects the cervical levels) | Composed of osteoblasts that produce osteoid and fibrous bone |
| Giant cell tumour | 40-50yrs, more common in females | Over-expression in RANK/RANKL signalling pathway, resulting in over-proliferation of osteoclasts |
Primary Malignant Tumours
|
Tumour Subtype |
Demographic Most Affected |
Pathogenesis |
| Osteosarcoma | 30-50yrs, more common in males (mostly affects the lumbosacral levels) | A mesodermally derived lesion producing osteoid tissue |
| Chondrosarcoma | 40-60yrs (mostly affects the thoracic levels) | Histology often shows the hyaline cartilage with increased cellularity within a myxoid matrix |
| Chordoma | 30-50yrs (mostly affects the sacrum) | Soft tissue lobulated mass with mucinous cells that extend into adjacent vertebra |
| Multiple myeloma | 50yrs+ (mostly affects the lumbosacral levels) | Arises from the plasma cells on the reticular stroma |
| Ewing sarcoma | 20-30yrs (mostly affects the lumbosacral levels) | Composed of small round blue cells, it arises from the medullary cavity with invasion of the Harvesian system |
Intramedullary
| Tumour Subtype | Demographic Most Affected |
Pathogenesis |
| Ependymoma | 30-50yrs, more common in males | Arise from ependymal cells lining the central canal; perivascular pseudorosettes (collection of tumour cells around a blood vessel) are often observed |
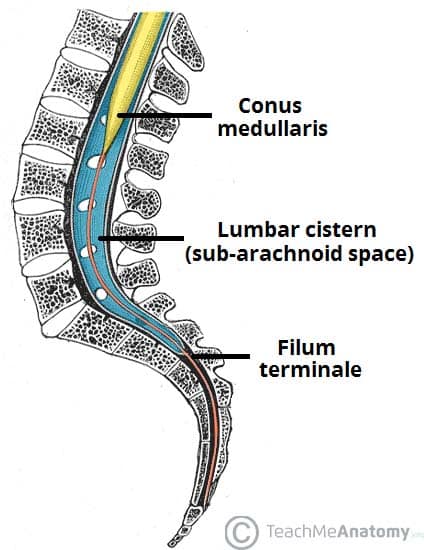
| Myxopapillary ependymoma
|
30-50yrs, more common in males | Arise from the ependymal glial cells, almost exclusively at the conus medullaris and filum terminale
|
| Astrocytoma | 20-40yrs, more common in males | Malignant tumour from the astrocytes (albeit, majority of astrocytomas are benign) |
| Hemangioblastoma
|
30-50yrs, more common in males. Associated with von Hippel Lindau disease | Vascular tumours, composed of endothelial cells, pericytes and stromal cells |
Extramedullary
| Tumour Subtype | Demographic Most Affected | Pathogenesis |
| Nerve sheath tumours | 30-50yrs, associated with neurofibromatosis | Arise from nerve sheath cells around the spinal roots |
| Meningioma | 50-70yrs, more common in females (mostly affects the thoracic levels) | Arise from arachnoid villi cells, generally slow-growing lesions |