This article is for educational purposes only. It should not be used as a template for consenting patients. The person obtaining consent should have clear knowledge of the procedure and the potential risks and complications. Always refer to your local or national guidelines, and the applicable and appropriate law in your jurisdiction governing patient consent.
Overview of Procedure
The common femoral artery is particularly susceptible to stenosis, and is typically poorly treated through endovascular means. Thus, common femoral endarterectomy is a frequently performed procedure.
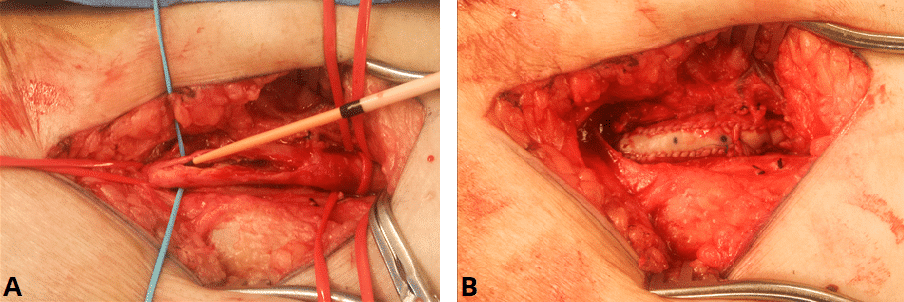
It involves dissection of the common femoral artery and its bifurcation into the superficial femoral artery and profunda artery. These are slung and clamped where the artery becomes healthy again, with the artery opened longitudinally and the atherosclerotic plaque excised from the arterial media.
The artery is typically closed with a bovine patch to avoid stenosis in the artery from primary closure.
Complications
Intraoperative
| Complication | Description of Complication | Potential Ways to Reduce Risk |
| Haemorrhage | This can occur due to damage to either the artery or the femoral vein or its branches, and may require blood transfusion. | |
| Injury to surrounding structures including femoral nerve or vein | The femoral artery lies between the femoral nerve and femoral vein. Either of these can be damaged during the dissection if not careful. | Dissect using a standard approach with identification of the inguinal ligament primarily, then approach the artery proximally |
| Anaesthetic risks | Includes damage to the teeth, throat and larynx, reaction to medications, nausea and vomiting, cardiovascular and respiratory complications. | Forms a part of the anaesthetist assessment before the operation |
Early
| Complication | Description of Complication | Potential Ways to Reduce Risk |
| Pain | The patient will most likely have an epidural anaesthetic to minimise pain. | |
| Bleeding | There is a small chance of bleeding and bruising in the abdomen post-operatively. | |
| Infection | Superficial wound infection is possible, yet graft infections are also possible and are major complication that require life-long antibiotics and graft excision if possible. | Peri-operative antibiotics will reduce the risk of wound and graft infections |
| Scarring | A longitudinal or transverse incisions will result in a scar, which may form a keloid scar, particular in high risk ethnicities. | |
| Seroma | A swelling of lymphatic fluid may occur particularly in the groin due to disruption of the lymph nodes and channels. | Careful dissection of the lymphatic nodes and channels with ligation will minimise this risk. |
| Blood clots | DVTs and PEs are a possibility in any operation. The risk is increased in patients with a raised BMI, on the pill, recent flights, previous DVT, pregnancy, smokers, cancer and prolonged bed rest. | The patient will be given anti-embolism stocking and low molecular weight heparin peri-operatively to minimise this risk as deemed appropriate. |
| Compartment syndrome | Compartment syndrome may occur in patients with prolonged clamp times or in the acute setting. Patients with a long history of peripheral vascular disease are preconditioned for ischaemia so it is less likely to occur in such patients | Minimise clamp times |
| Stroke, MI, kidney failure, death | Although small, this is always a risk in any major surgery |
Late
| Complication | Description of Complication | Potential Ways to Reduce Risk |
| Hernia | Any groin incision can cause a hernia if there is damage to the inguinal ligament or extensive lifting of the ligament during the procedure. | |
| Reintervention | The common femoral artery may become stenosed again over time, requiring a redo procedure, or more proximal or distal disease may necessitate a bypass in the future. |