Introduction
A volvulus is a twisting of a loop of bowel around its mesenteric attachment. The word volvulus derives from the Latin “to twist”
A volvulus is a surgical emergency. A closed loop bowel obstruction forms within the affected segment of bowel and the twisting causes a compromise to the blood supply, rapidly leading to bowel necrosis and perforation.
Most volvuli occur at the sigmoid colon, due to its long mesentery making it prone to twist (especially with increasing age), making it a common cause of large bowel obstruction. Other sites of volvulus include the stomach, caecum, small intestine and transverse colon, but these are much rarer.
This article will mainly focus on the risk factors, clinical presentation, and management of a sigmoid volvulus.
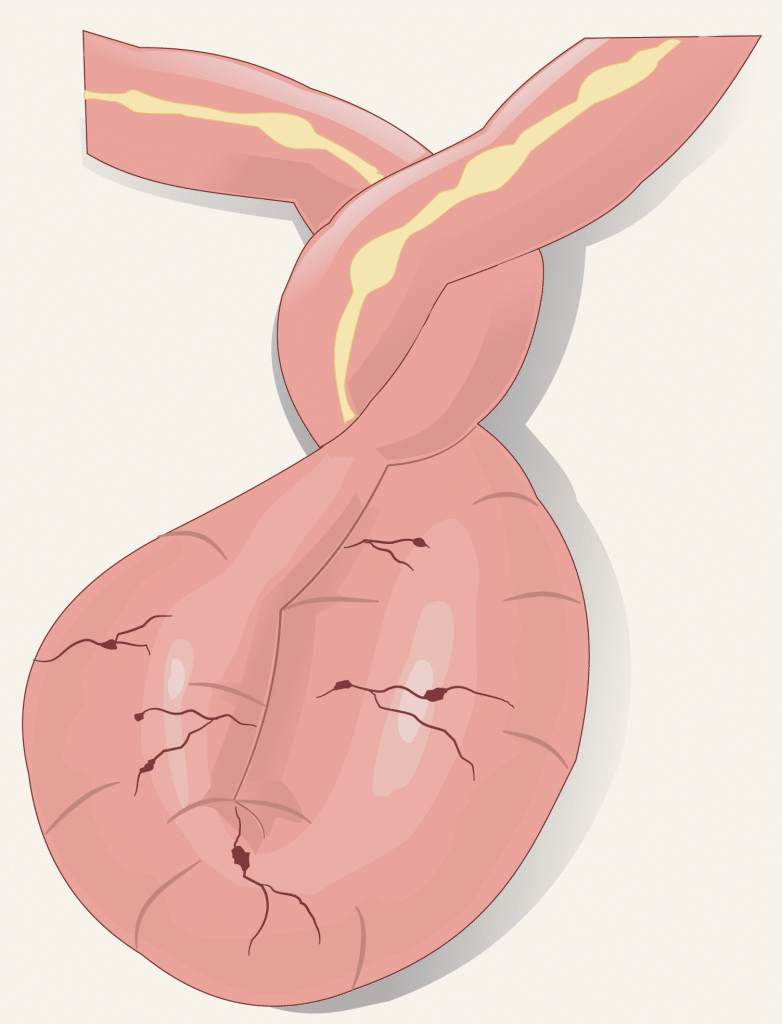
Figure 1 – A volvulus occurs when bowel twists on its own mesentery
Risk Factors
The main risk factors for sigmoid volvulus include advanced age, neurological disorders (e.g. Parkinson’s disease or vascular dementia), psychiatric disease (those on anti-psychotics in particular), patients with reduced mobility, and male gender.
All these risk factors increase the chance of patients having chronic constipation and slow-transit gastrointestinal tracts. This, in turn, results in patients developing a redundant sigmoid colon, which then becomes prone to twisting.
Clinical Features
Patients with a sigmoid volvulus will typically present with abdominal distension and absolute constipation, with varying degrees of abdominal pain. If left untreated, this will then result in vomiting, secondary to the bowel obstruction
Particularly noteworthy in cases of volvulus, compared to other causes of bowel obstruction, is the rapidity of its onset (over a few hours) and the degree of abdominal distension.
On examination, the abdomen is distended and tympanic to percussion. Whilst patients may have localised tenderness, any features of peritonism are concerning for developing bowel ischaemia.
Differential Diagnosis
The main differential diagnoses to consider large bowel obstruction secondary to a diverticular stricture or colorectal cancer, or pseudo-obstruction.
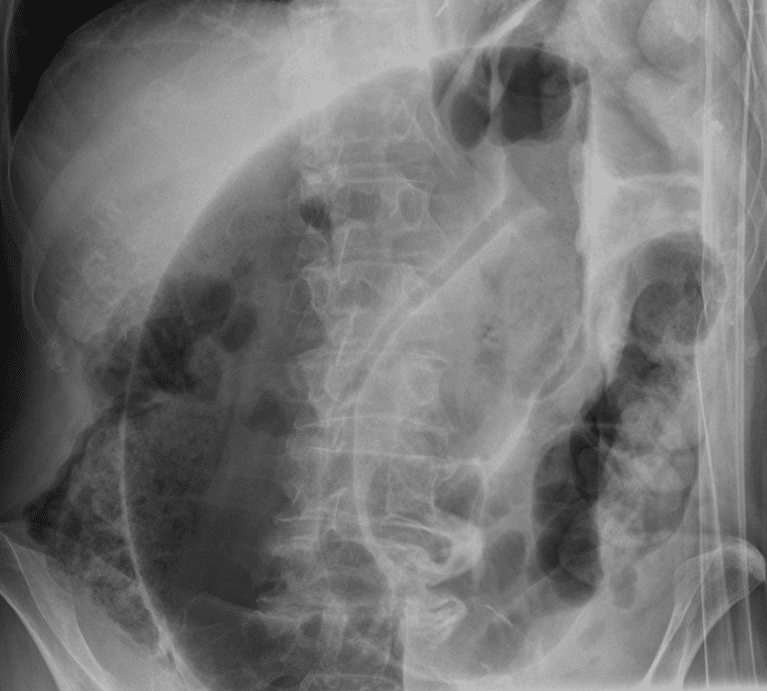
Figure 2 – A plain film abdominal radiograph (AXR) showing a sigmoid volvulus
Investigations
All patients with suspected sigmoid volvulus should have urgent blood tests performed, including FBC, U&Es, CRP, and clotting screen. A venous blood gas should be performed to check pH and serum lactate, in the context of potential bowel ischaemia.
The definitive diagnosis requires a CT abdomen-pelvis scan with intravenous contrast. CT imaging will demonstrate a very dilated sigmoid colon with an associated “whirl sign” (Fig. 3), where the twist within the mesentery is visualised around its base.
CT imaging is useful to also assess for any radiological evidence of bowel ischaemia. If the ileocaecal valve is incompetent, there will also be radiological signs of small bowel obstruction.
Whilst less sensitive, plain-film abdominal radiographs (AXR) are often used a first line imaging; this will classically show (in around 60-75% cases) a “coffee-bean sign” arising from the left iliac fossa (Fig. 2).
Figure 3 – A CT scan demonstrating a sigmoid volvulus, with a “whirl sign” in the mesentery
Management
All patients presenting with a sigmoid volvulus are often intravascularly fluid deplete therefore need aggressive fluid resuscitation.
Ensure a nasogastric tube is placed, especially if the patient is vomiting, and a urinary catheter is inserted for fluid balance assessment. Adequate analgesia should be prescribed and ensure any electrolyte abnormalities are corrected.
Conservative Management
Most patients with sigmoid volvulus are treated conservatively initially with decompression by sigmoidoscope and insertion of a flatus tube.
In sigmoidoscope decompression, the patient is placed in the left lateral position and a lubricated sigmoidoscope gently guided into the rectum. It is manoeuvred to locate the twisted bowel and, with gentle pressure, the volvulus can be untwisted – once the sigmoidoscope is in the correct position, there will be a rush of air and liquid faeces as the obstruction is relieved.
A flatus tube is often left in situ for a period of time (up to 24 hours) after initial decompression to allow for the continued passage of contents and aid recovery of the affected area.
In a significant proportion of patients, decompression with a rigid sigmoidoscope cannot be successfully achieved and a formal flexible sigmoidoscopy is required.
Surgical Management
Emergency surgery is required for patients with a sigmoid volvulus in those with any evidence of bowel ischaemia or perforation (or in those with repeat failed endoscopic decompression).
This will require the patient to undergo a sigmoid colectomy, often as a laparotomy and Hartmann’s procedure (given the patient cohort is typically co-morbid and frail, a resection and primary anastomosis is not usually advised).
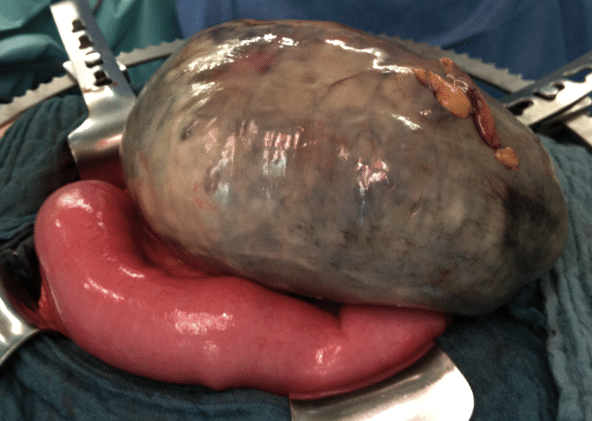
Figure 4 – A sigmoid volvulus with ischaemic bowel, warranting a surgical resection
Patients with recurrent volvulus may choose to have an elective procedure, either as a sigmoid colectomy with primary anastomosis or end colostomy, to prevent further recurrence. The risks of recurrence need to be balanced against the risks of surgery, especially in this often frail and co-morbid patient group.
Complications
The main immediate complication of a sigmoid volvulus is of bowel ischaemia and perforation. Longer term complications are mainly the risk of recurrence (occurring in up to 90% of patients)
Caecal Volvulus
The second most common site for a volvulus to occur is at the caecum, accounting for around 25-40% of all colonic volvulus. There is a bimodal age of onset, in the 10-29 year group and again in the 60-79 year group.
Those in the younger group may have intestinal malformation (or less commonly from excessive exercise) as the predisposing cause, whilst in older patients the risk factors are similar for sigmoid volvulus.
Diagnosis is once again made on CT imaging, which shows a very distended caecum, a mesenteric “swirl” and small bowel obstruction. The management of a caecal volvulus requires a bowel resection, typically a right hemicolectomy.
Key Points
- A volvulus is a twist in the bowel, most commonly occurring at the sigmoid colon
- Risk factors include advanced age, neurological disorders, psychiatric disease, and those with reduced mobility
- Diagnosis is typically made either via plain film abdominal radiographs or CT imaging
- Initial management warrants endoscopic decompression and flatus tube insertion
