Introduction
Epicondylitis is a symptomatic chronic inflammatory condition of the forearm tendons at the elbow.
It is an overuse syndrome in the elbow. It is caused by microtears in the tendons attaching to the epicondyles of the elbow following repetitive injury. It affects males and females equally, with a peak onset between 35-54 years old.
There are two types commonly described: lateral epicondylitis (or “Tennis elbow”) and medial epicondylitis (or “Golfer’s elbow”). Lateral epicondylitis is the more common, affecting 4-7 people per 1000 per year.
This article predominantly focuses on lateral epicondylitis, with medial epicondylitis described at the end of this article.
Pathophysiology
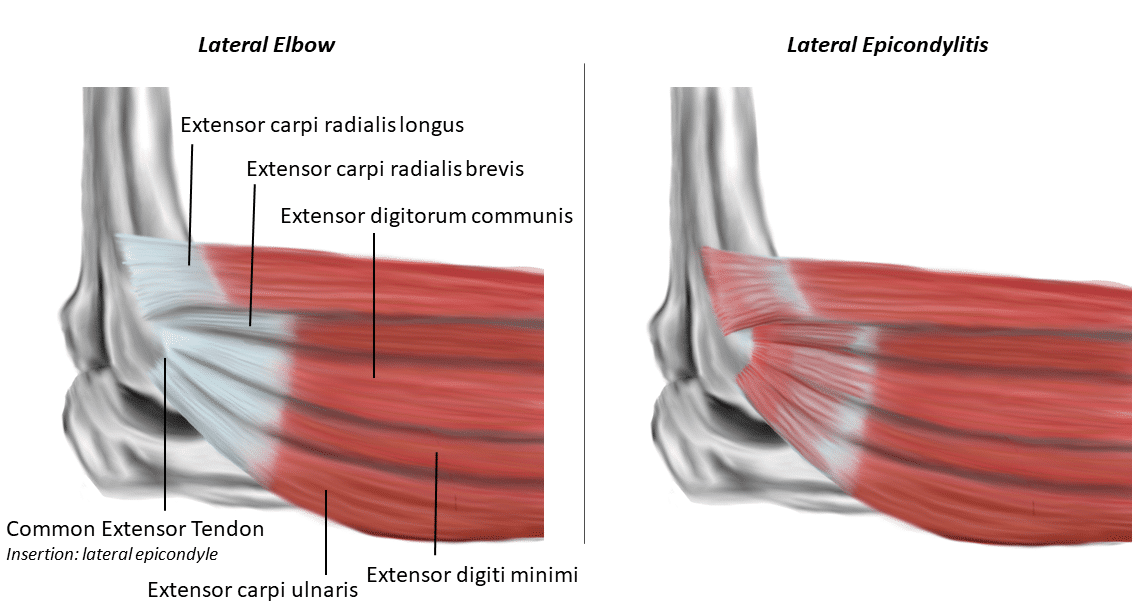
The medial and lateral epicondyles are small bony tuberosities on the distal end of the humerus (Fig. 1). The common extensor tendon attaches to the lateral epicondyle, acting as the common attachment for the superficial extensor muscles of the forearm.
Repetitive overuse of the tendons can cause microtears in the tendon at their origin; the tendon adapts to the multiple tears, leading to the formation of granulation tissue, fibrosis and eventually tendinosis.
Risk Factors
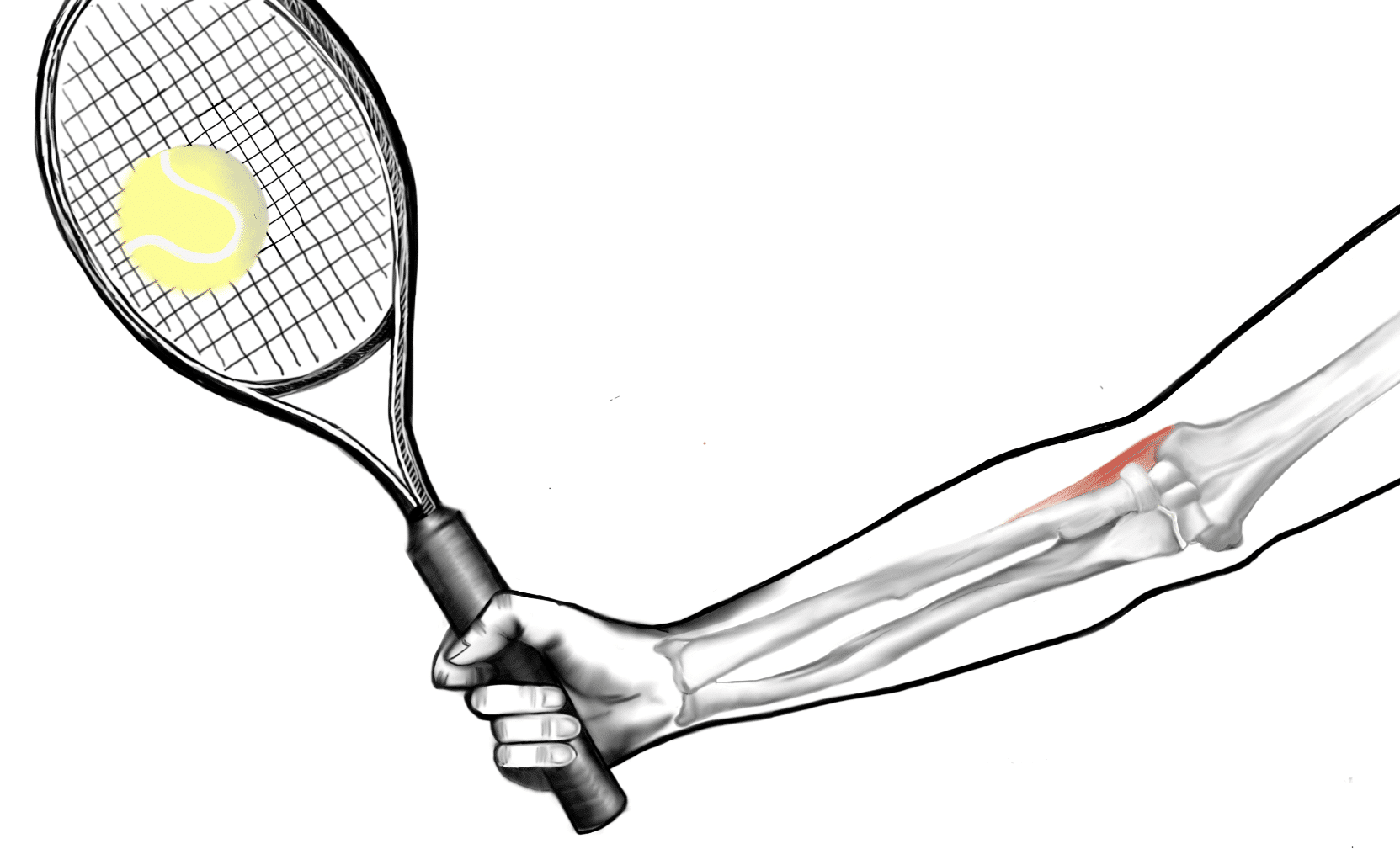
The main risk factors for lateral epicondylitis are those occupations and hobbies that are associated with excessive repetitive use of extensor forearm muscles (such as tennis).
Clinical Features
The main symptom of epicondylitis is pain affecting the elbow and radiating down the forearm. The pain typically worsens over weeks to months, most often affecting the dominant arm. Motor function and sensation of the upper limb will otherwise be unaffected.
On examination, patients will have local tenderness on palpation over (or distal to) the lateral epicondyle and common extensor tendon. Due to the pain, there may be a reduced grip strength, with a full range of movements at the wrist and the elbow.
Special Tests for Lateral Epicondylitis
Two specific tests for lateral epicondylitis can be performed to further elucidate the diagnosis, both tests being positive if pain is felt during the respective manoeuvres:
- Cozen’s Test – The patient’s elbow is held flexed to 90 degrees, with one examiner’s hand held over the lateral epicondyle, whilst the other hand holds the patient’s hand in a radially deviated position with the forearm pronated; the patient is then asked to extend their wrist against resistance
- Mill’s Test – The patient’s lateral epicondyle is palpated by the examiner, whilst also pronating the patient’s forearm, flexing the wrist, and extending the elbow
Differential Diagnoses
- Cervical radiculopathy – often associated with neck pain and stiffness, as well as a sensorimotor deficit in the affected dermatome or myotome
- Elbow osteoarthritis – joint stiffness, worse towards the end of the day, associated with reduced range of movement and end-range pain
- Radial carpal tunnel syndrome – maximal tenderness is localised to area distal to radial head (rather than the lateral epicondyle), with pain on thumb and index finger extension
Investigations
The diagnosis is typically clinical. However, in unclear cases or those resistant to treatment, ultrasound or MRI imaging (Fig. 3) can be used to confirm the diagnosis or to detect any structural abnormality.
Management
Patients should be advised to modify their activities, reducing the repetitive actions causing the condition. Simple analgesics alongside topical NSAIDs should be prescribed to help with the pain.
If symptoms persist despite this, corticosteroid injections can be administered, injected into the region around the tendon and can be repeated every 3-6 months.
Physiotherapy can provide longer term relief via stretching and strengthening exercises for wrist and forearm extensors. Orthoses (a wrist or elbow brace) can be used in conjunction with physiotherapy for potential longer-term symptom relief.
Surgical Treatment
Referral to an orthopaedic surgeon may be warranted if the symptoms are not controlled through conservative measures.
Open or arthroscopic debridement of tendinosis and release or repair of any damaged tendon insertions may be required. If the tendon has more than 50% damage, tendon transfer may be required to ensure function is retained.
Prognosis
Lateral epicondylitis is self-limiting and spontaneously improves in 80-90% of people in 1-2 years.
Medial Epicondylitis
Medial epicondylitis, also known as ‘Golfer’s elbow’, is a similar condition, affecting the tendons that attach to the medial epicondyle of the humerus (the flexors). In medial epicondylitis, pronator teres and flexor carpi radialis are the most commonly affected tendons.
When examining, these patients will have tenderness over pronator teres and flexor carpi radialis tendons. The treatment for medial epicondylitis is the same as the course of treatment for lateral epicondylitis.
Key Points
- Epicondylitis is caused by microtears in the tendons attaching to the epicondyles of the elbow following repetitive injury
- The main feature is pain affecting the elbow and radiating down the forearm
- Analgesia, lifestyle modification, and physiotherapy form the mainstay of management
- In unremitting or severe cases, debridement of tendinosis and release or repair of any damaged tendon insertions may be required